Injectable Oxygen set to make resuscitation easier and safer...
AED Drone bringing help to the scene before ambulance arrival...
Why We Should No Longer Terminate Resuscitations after 20 Minutes...<click here>
Research shows defibrillation depicted in movies is far from accurate <click here>
The truth is out there...

While it is recognised around the world that the most common cardiac arrest is the Sudden Cardiac Arrest (SCA)...here in Australia we act as if the the most common arrest is in an adult who drowns while eating a meat pie. Very Australian but just not true!? See our discussion page and check out the facts.
Dr Heimlich saves choking woman with man-oeuvre he invented
The 96-year-old American inventor of the Heimlich manoeuvre has used the technique himself to save a choking woman at his retirement home. Dr Henry Heimlich said he had demonstrated the technique many times but never used it in an emergency. His action dislodged a piece of meat with a bone in it from the 87-year-old woman's airway. "I didn't know I really could do it until the other day," he told the BBC. Dr Heimlich was having dinner with eight or nine others at the Deupree House retirement home in Cincinnati when he turned to talk to a woman at his table and noticed she was choking. "She had a skin colour that was no longer pink. Her mouth was puffed up and her lips were out," he told the BBC. "Though I invented the Heimlich manoeuvre I had never been called on to do it before." Dr Heimlich described how he turned the woman, Patty Ris, around in her chair so her back was exposed. The manoeuvre requires a rescuer to carry out abdominal thrusts on a choke victim to dislodge the blockage. "I did it three times and a piece of meat with a bone in it came flying out of her mouth and she was all right," he said. Staff had rushed to the table when the woman started choking, but stood back to allow Dr Heimlich to carry out his manoeuvre. "Just the fact that a 96-year-old man could perform that, is impressive," his son Phil Heimlich told the Cincinnati Inquirer. Dr Heimlich, who invented the technique in 1974, swims and exercises regularly. He often meets people who were saved by the technique or who saved someone else, his son said.
Who has the Heimlich manoeuvre saved? Since the technique was introduced in 1974 it is believed to have saved the lives of more than 100,000 people in the US alone. They include former President Ronald Reagan, pop star Cher, former New York mayor Edward Koch and Hollywood actors Elizabeth Taylor, Goldie Hawn, Walter Matthau, Carrie Fisher, Jack Lemmon and Marlene Dietrich. In 2014 actor Clint Eastwood was credited with saving the life of a golf tournament director in California who was choking on a piece of cheese. In the UK, celebrity promoter Simon Cowell was reportedly saved by comedian David Walliams, who carried out the Heimlich manoeuvre on him after a mint became stuck in his throat.
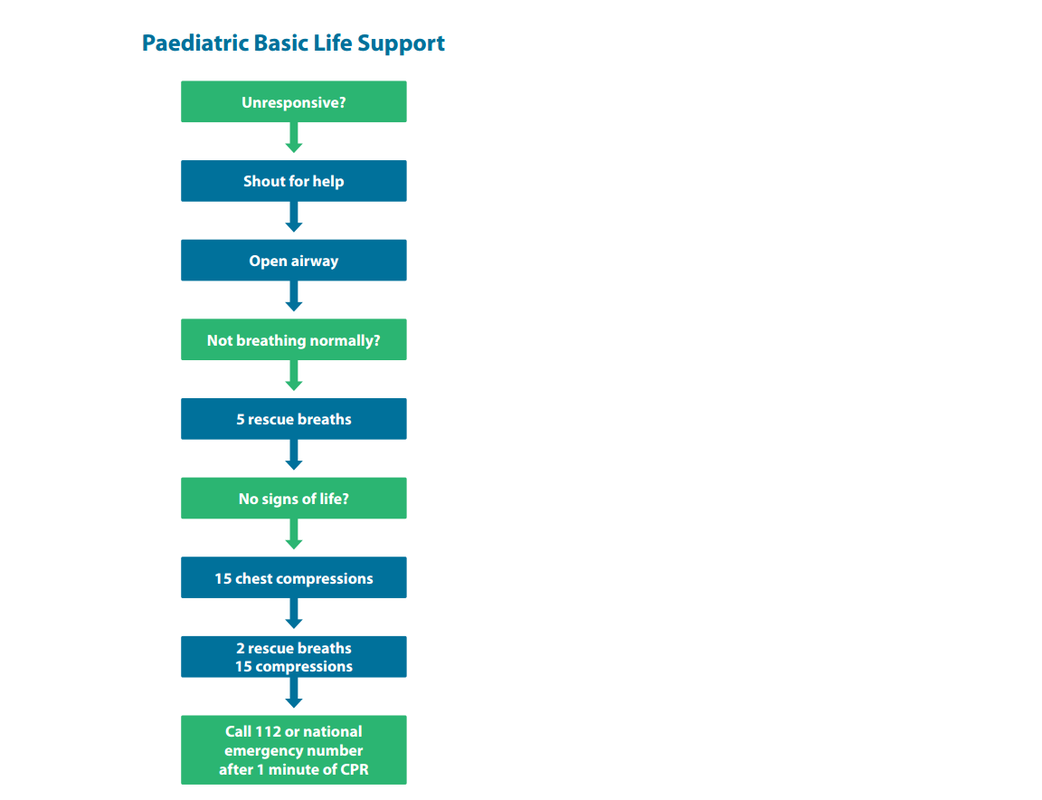
European Resuscitation Council releases new guidelines
The European Resuscitation Council (ERC) has released their new guidelines, including now recommending that the BLS Guidelines for Children be the same as the ALS Guidelines (see below). This includes using the ratio of 15:2 for CPR due to the high likelihood that a peadiatric arrest will by caused by a hypoxic episode.
The European Resuscitation Council (ERC) has released their new guidelines, including now recommending that the BLS Guidelines for Children be the same as the ALS Guidelines (see below). This includes using the ratio of 15:2 for CPR due to the high likelihood that a peadiatric arrest will by caused by a hypoxic episode.
ECC and AHA recommend first-aiders and other BLS providers are given Naloxone (Narcan) for narcotic over-doses
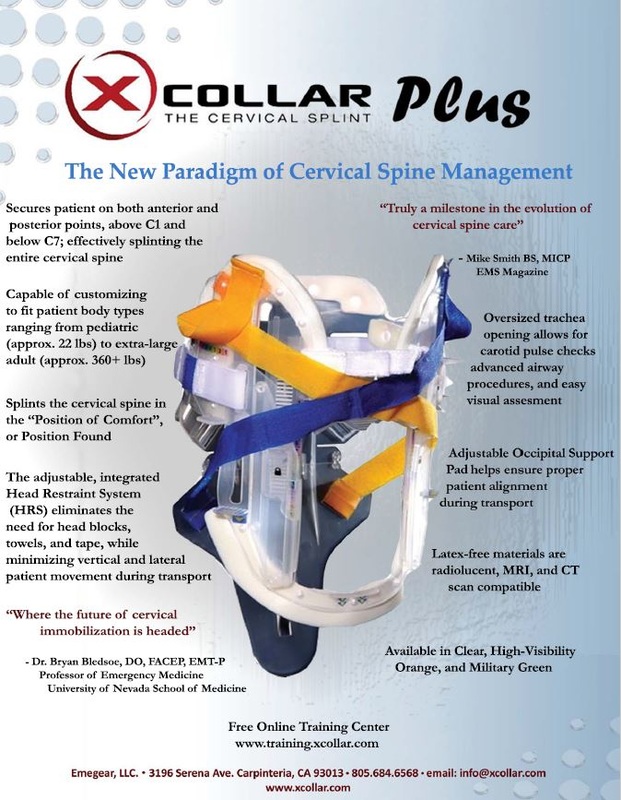
New Collars solves the issues for the critics of hard collars
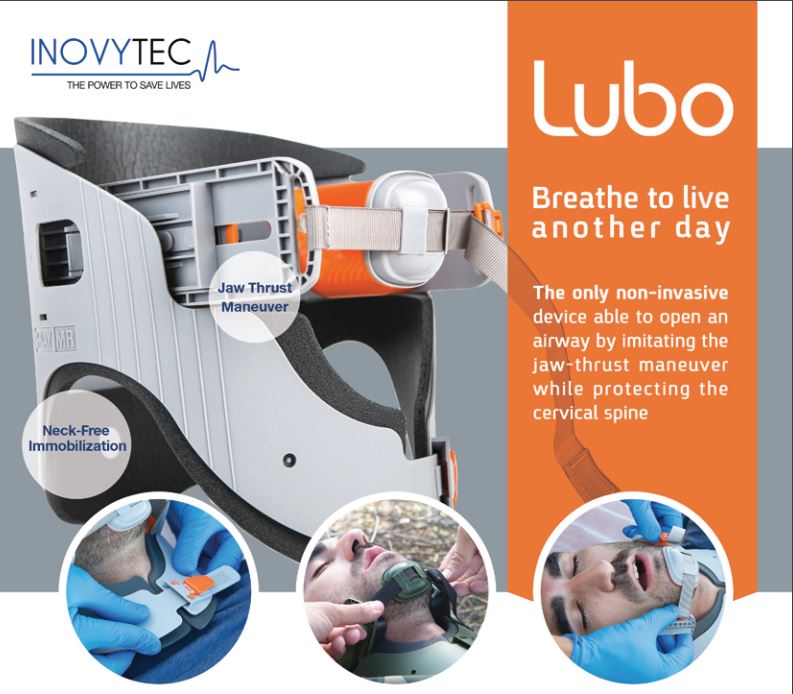
The Lubo
The Lubo offers a combined solution for both airway and immobilization needs. While the Lubo is the only non-invasive solution that can safely open the airway by imitating the jaw thrust maneuver for a long time, it is the only immobilization device that allows the care giver to manage the airway easily, frees the neck from the “traditional neck grasp” while performing solid immobilization.
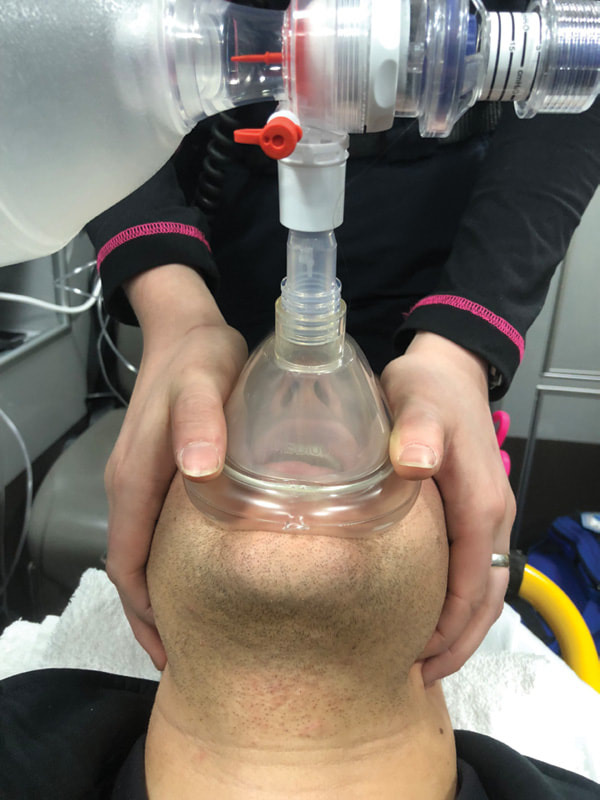
Any first responder, paramedic or non-paramedic, learns in the Basic Life Support course to perform the Jaw-thrust maneuver using both hands.
On the one hand, this is a difficult technique that requires training in order to be performed successfully, and still may risk the patient’s cervical spine if done manually without preliminary immobilization. On the other hand, the common cervical collars may compromise the patient’s airway by obstructing both the professional medical personnel from performing intubation and the Basic Life Support first responders from manually performing a Jaw-thrust maneuver.
The Lubo offers a combined solution for both airway and immobilization needs. While the Lubo is the only non-invasive solution that can safely open the airway by imitating the jaw thrust maneuver for a long time, it is the only immobilization device that allows the care giver to manage the airway easily, frees the neck from the “traditional neck grasp” while performing solid immobilization.
Any first responder, paramedic or non-paramedic, learns in the Basic Life Support course to perform the Jaw-thrust maneuver using both hands.
On the one hand, this is a difficult technique that requires training in order to be performed successfully, and still may risk the patient’s cervical spine if done manually without preliminary immobilization. On the other hand, the common cervical collars may compromise the patient’s airway by obstructing both the professional medical personnel from performing intubation and the Basic Life Support first responders from manually performing a Jaw-thrust maneuver.
Lubo secures patent airway while immobilizing the spine without causing damage to the patient’s neck. Lubo also enables performing intubation, if needed, while maintaining cervical spine fixation.
Lubo meets the first-aid international guidelines, both civilian and military, allowing basic patent airway and can quickly be applied by any first responder. The Lubo can easily be included in any first-aid kit and therefore improve health and wellness in the community.
Lubo sales commenced worldwide through distributors specialized in out-of-hospital emergencies both to the civil (private and government) and military markets.
History
The Lubo stems from field experience in the Israeli Army (IDF). The inventor, Dr. Omri Lubovski, is a veteran in the prestige aviation rescue 669 unit. He realized that the need for opening the airway non-invasively, quickly and efficiently, is crucial especially when the victim’s situation or scene surroundings are complicated. The lack of ability to open and secure the patient’s airway while performing immobilization, led to the invention of Lubo.
The Need
The Lubo concept has grown out of two major needs in the field of emergency medicine:
This novel device is intended to enable non-invasive airway management in cases of trauma that require immediate airway management combined with an immobilization capability1.
Lubo’s main features
Lubo Family Models:
The Lubo family includes various models addressing the need to open and secure patent airway by any first responder in different segments of the critical care market, such as emergency services, first-aid kits, hospital ER/ICU, military and MCI.
Lubo Regular
Enables patented airway opening with cervical spine immobilization, adjustable to adult sizes, single-use for pre-hospital medical emergency care.
Lubo Military Model
Enables patented airway opening with cervical spine immobilization, adjustable to adult sizes for use by military forces. Robust, dark colors, for pre-hospital use, complied with TCCC and TEMP guidelines.
Lubo Mini
Enables patented airway opening with cervical spine immobilization, adjustable to small sizes, single-use for pre-hospital medical emergency care.
References:
Lubo meets the first-aid international guidelines, both civilian and military, allowing basic patent airway and can quickly be applied by any first responder. The Lubo can easily be included in any first-aid kit and therefore improve health and wellness in the community.
Lubo sales commenced worldwide through distributors specialized in out-of-hospital emergencies both to the civil (private and government) and military markets.
History
The Lubo stems from field experience in the Israeli Army (IDF). The inventor, Dr. Omri Lubovski, is a veteran in the prestige aviation rescue 669 unit. He realized that the need for opening the airway non-invasively, quickly and efficiently, is crucial especially when the victim’s situation or scene surroundings are complicated. The lack of ability to open and secure the patient’s airway while performing immobilization, led to the invention of Lubo.
The Need
The Lubo concept has grown out of two major needs in the field of emergency medicine:
- Non-invasive airway solution
- Cervical collars pitfalls
This novel device is intended to enable non-invasive airway management in cases of trauma that require immediate airway management combined with an immobilization capability1.
Lubo’s main features
- Non-invasive airway management.
- Imitates the jaw thrust maneuver while protecting the cervical spine. Performs a safer jaw thrust maneuver without risking the spine6.
- Avoids using ‘invasive’ airway devices OPAs (which can result in pallet trauma, nausea, vomiting and bronco-aspiration) and NPAs (which may lead to bleeding).
- Facilitates airway clearance (teeth, secretions etc.).
- Immobilization without compromising the airway and without grasping the neck.
- The only cervical collar that enables intubation (no need to remove the collar) and its immobilization is at least as good as the standard cervical collars.
- Easy to operate by any first-responders.
- Effective, fast and painless.
Lubo Family Models:
The Lubo family includes various models addressing the need to open and secure patent airway by any first responder in different segments of the critical care market, such as emergency services, first-aid kits, hospital ER/ICU, military and MCI.
Lubo Regular
Enables patented airway opening with cervical spine immobilization, adjustable to adult sizes, single-use for pre-hospital medical emergency care.
Lubo Military Model
Enables patented airway opening with cervical spine immobilization, adjustable to adult sizes for use by military forces. Robust, dark colors, for pre-hospital use, complied with TCCC and TEMP guidelines.
Lubo Mini
Enables patented airway opening with cervical spine immobilization, adjustable to small sizes, single-use for pre-hospital medical emergency care.
References:
- Lubovsky, O., Liebergall, M., Weissman, C. & Yuval, M. A new external upper airway opening device combined with a cervical collar. Resuscitation 81, 817–821 (2010).
- Lairet, J. R. et al. Prehospital interventions performed in a combat zone. J. Trauma Acute Care Surg. 73, S38–S42 (2012).
- Eastridge, B. J. et al. Death on the battlefield (2001–2011). J. Trauma Acute Care Surg. 73, S431–S437 (2012).
- Uzun, L. et al. Effectiveness of the jaw-thrust maneuver in opening the airway: A flexible fiberoptic endoscopic study. ORL 67, 39–44 (2005).
- Durga, V. K., Millns, J. P. & Smith, J. E. Manoeuvres used to clear the airway during fibreoptic intubation. Br. J. Anaesth. 87, 207–211 (2001).
- Aprahamian, C. et al. Experimental Cervical Spine Injury Model : Evaluation of Airway Management and Splinting Techniques. (1984).
- Goutcher, C. M. & Lochhead, V. Reduction in mouth opening with semi-rigid cervical collars. Br. J. Anaesth. 95, 344–348 (2005).
- George, J. W., Fennema, J., Maddox, A., Nessler, M. & Skaggs, C. D. The effect of cervical spine manual therapy on normal mouth opening in asymptomatic subjects. J. Chiropr. Med. 6, 141–145 (2007).
- Benger, J. & Blackham, J. Why do we put cervical collars on conscious trauma patients? Scand. J. Trauma. Resusc. Emerg. Med.17, 44 (2009).
- Sundstrøm, T., Asbjørnsen, H., Habiba, S., Sunde, G. A. & Wester, K. Prehospital use of cervical collars in trauma patients: a critical review. J. Neurotrauma 31, 531–40 (2014).
The X Collar |
Who will win the "Australian - Fast Food AED Challenge"
A challenge open to all the major fast food chains in Australia. Be the first to install defibrillators (AED's) in your restaurants and get bragging rights.
With such huge profits being made in Australia by fast food companies and the importance of a balanced approach to food intake, now is the time for these retailers (who share 51.5 million visits a year in Australia) to show leadership in customer care and install defibrillators (AED's) in all their restaurants. This will help address the biggest single killer of Australians, Sudden Cardiac Arrest (SCA). Survival is less than 10% without an AED and up to 75% if the first shock is delivered in the first 3 minutes i.e. before Ambulance arrival.
With such huge profits being made in Australia by fast food companies and the importance of a balanced approach to food intake, now is the time for these retailers (who share 51.5 million visits a year in Australia) to show leadership in customer care and install defibrillators (AED's) in all their restaurants. This will help address the biggest single killer of Australians, Sudden Cardiac Arrest (SCA). Survival is less than 10% without an AED and up to 75% if the first shock is delivered in the first 3 minutes i.e. before Ambulance arrival.
"Hands only" CPR improves bystander willingness to start resuscitation by 70% in Sweden but in Australia bystanders are still encouraged to use "rescue breaths" in all resuscitation attempts?!
NEW ORLEANS – Since guidelines have endorsed the use of compression-only or Hands-Only CPR by people not trained or unwilling to provide rescue breaths during resuscitation attempts, Swedish bystanders are trying to help at a far greater rate.
Using a national registry in Sweden of 23,169 bystander-witnessed cases of out-of-hospital cardiac arrest, researchers compared the total rate of bystander CPR attempted and the proportions of standard CPR , which involves both rescue breaths and chest compressions; and Hands-Only CPR.
They found: Bystanders attempted to resuscitate a total of 38 percent of people in cardiac arrest from 2000-2005 — before compressions-only-CPR was introduced into the guidelines. During 2006-2010 — after guidelines noted that dispatcher guidance of laypeople in compressions-only CPR might be preferable — 59 percent of bystanders attempted resuscitation CPR. The total rate of CPR attempts rose to 70 percent during 2011-2014, after guidelines strongly recommended that dispatchers instruct untrained bystanders in compressions-only-CPR.
Most of the increase in bystander CPR during the last 15 years in Sweden was associated with increased use of compressions-only-CPR, from 5 percent in 2000-2005 to 15 percent in 2006-2010 to 28 percent in 2011-2014. The 30-day survival of people with out-of-hospital cardiac arrest was not significantly different between those receiving compressions-only-CPR (13.6 percent) and standard CPR (12.9 percent). Either approach resulted in far higher survival than when no CPR was attempted (6.4 percent during 2011-2014).
The study was presented Saturday at the Resuscitation Science Symposium taking place at American Heart Association’s Scientific Sessions 2016.
An important lesson for the NSW Government on its attitude to AEDs in schools. Creating a regulatory framework is not removing barriers for schools wanting to purchase an AED!
|
Teachers save teenager's life after he goes into cardiac arrest at school
By MattJarram | Posted: December 13, 2016 - Nottingham Post A Nottinghamshire mum says quick-thinking staff saved her 17-year-old son's life after he suffered a sudden cardiac arrest while at school. Sarah Walker, 52, of Lingford, Cotgrave, says that if it wasn't for staff at South Nottinghamshire Academy, her son, Charlie Allison, would not be with them today. The keen Nottingham Forest supporter suddenly collapsed at 2.30pm on Friday while exercising in the school's Fitness Suite. The sports-mad pupil, who plays football for Bingham Town, had suffered a sudden cardiac arrest – and every moment was critical as school staff fought to save his life. The Radcliffe-on-Trent school has a defibrillator on site – which delivers a charge to the heart – and had just received whole school training on how to use the defib a week before Charlie collapsed. PE teacher, Scott Lowman, 31, and inclusion manager, Sam Proctor, 43, rushed to Charlie's aid and managed to bring the young lad back to life. The pair, assisted by pupils and staff, managed to start Charlie's heart before a road ambulance and the air ambulance arrived on site. Charlie's mother, Sarah Walker told the Post: "We owe the school Charlie's life. They gave us our son back. Without them I would not have a son. There is no doubt. Without the defibrillator he would not have made it to the hospital." In fact, the school said that Charlie, who is now recovering on the Acute Cardiac Ward at the City Hospital, was apparently most upset because his Nottingham Forest shirt had to be cut off while they worked on his heart. Explaining the ordeal, PE teacher Scott Lowman, who helped to save Charlie's life, told the Post: "One of the young lads in the fitness suite came running out and said Charlie had fainted. It was a scary situation. He started to go downhill – his breathing slowed and at one point stopped. "We shouted for the defibrillator after noticing his heart had stopped and I started CPR while waiting for the defibrillator. We delivered the shot which started Charlie's heart again. I am still struggling to come to terms with what has happened. Without the defibrillator he would not be here." Sam Proctor, who operated the defibrillator, added: "All of the school staff need praise. Everyone worked together to bring Charlie back to life." His mum says that Charlie has had no heart or breathing problems in the past and the family are anxiously waiting for a diagnosis following the close call. She said: "He is a fit and healthy boy. Charlie is a million miles away from where he was on Saturday and Sunday but he has a long way to recovery. We don't know what the diagnosis is yet. He is just a happy-go-lucky lad and very conscientious. Sport is his life and he lives and breathes sport." Charlie is undertaking a Level 3 Extended Diploma in Sport at the Academy in conjunction with Nottingham Forest. He has been a keen sportsman since he was six-years-old, making 144 appearances for Cotgrave Colts and playing for two years, mainly in right back, for Bingham Town. He is also in the Newark and Nottingham Cricket League for Keyworth Town and is a Nottingham Forest season ticket holder. Charlie has an older sister, Katie, 28. His mum, who is special needs teaching assistant at Oak Field School and Sports College, added: "I did not think I was ever going to see him again. Everyone went onto magic auto-pilot and brought him back to life." According to the British Heart Foundation, almost 90 percent of people who suffer out-of-hospital cardiac arrests die. The quick response was critical, as every minute without CPR and defibrillation reduces the chance of survival by up to 10 per cent. Dan Philpotts, head teacher at South Nottinghamshire Academy, said: "Our thoughts and best wishes are with Charlie and his family at this difficult time and we are so pleased to see him recovering in hospital. "Having seen first hand how a defibrillator helped saved Charlie's life, I cannot believe that they are not compulsory in schools and other public places. "South Nottinghamshire Academy staff were unbelievable and I am so proud of the way in which they responded – whilst it was very traumatic and some staff are struggling to come to terms with it, they can rest assured that they have contributed to saving a student's life." |
Stop Randomising all Cardiac Arrests
Myron L. Weisfeldt, MD
Read this paper from the American Heart Association's Circulation. 2016;134:2035-2036. on some of the issues with current and past cardiac arrest RCT research and the interpretration of outcomes. The author suggests that we may be missing important conclusions by randomizing all studies. <click here>
Public cardiopulmonary resuscitation training rates and awareness of hands-only cardiopulmonary resuscitation: a cross-sectional survey of Victorians.
Janet E Bray, Karen Smith, Rosalind Case, Susie Cartledge, Lahn Straney, Judith Finn
Emergency Medicine Australasia: EMA 2017 January 13
METHODS: A cross-sectional telephone survey in April 2016 of adult residents of the Australian state of Victoria was conducted. Primary outcomes were rates of CPR training and awareness of hands-only CPR.
RESULTS: Of the 404 adults surveyed (mean age 55 ± 17 years, 59% female, 73% metropolitan residents), 274 (68%) had undergone CPR training. Only 50% (n = 201) had heard of hands-only CPR, with most citing first-aid courses (41%) and media (36%) as sources of information.
RESULTS: Of the 404 adults surveyed (mean age 55 ± 17 years, 59% female, 73% metropolitan residents), 274 (68%) had undergone CPR training. Only 50% (n = 201) had heard of hands-only CPR, with most citing first-aid courses (41%) and media (36%) as sources of information.
ARAN Comment: The position taken by the ARC and its unofficial "spokespeople" ("unofficial", because the ARC refuses to debate the evidence with anyone outside their own organisation); is that the current DRSABCD appropriately prioritises compressions and defibrillation as the only two measures that have shown to make any difference in outcome in SCA in first response. The results of this study reinforce the position of ARAN; in that the message about compression-only CPR (which is the focus in all other jurisdictions in the world outside Australia and NZ) is not being articulated to the public in Australia. Half the population (even if they have been to a formal course or seen the propaganda from the ARC) have still not heard of compression only CPR being an alternative. All research on public willingness to help in an emergency shows an increased willingness if "rescue breaths" were omitted.
This survey would most likely have similar results in other states of Australia but will always show a huge variance to overseas, where the message is not hidden in an obsolete guideline for BLS (that is targeted to responding to hypoxic arrests). Another unfortunate (but predictable) fail from the ARC.
This survey would most likely have similar results in other states of Australia but will always show a huge variance to overseas, where the message is not hidden in an obsolete guideline for BLS (that is targeted to responding to hypoxic arrests). Another unfortunate (but predictable) fail from the ARC.
Association Between Tracheal Intubation During Adult In-Hospital Cardiac Arrest and Survival
Lars W Andersen, Asger Granfeldt, Clifton W Callaway, Steven M Bradley, Jasmeet Soar, Jerry P Nolan, Tobias Kurth, Michael W Donnino
JAMA: the Journal of the American Medical Association 2017 January 24
Importance: Tracheal intubation is common during adult in-hospital cardiac arrest, but little is known about the association between tracheal intubation and survival in this setting.
Objective: To determine whether tracheal intubation during adult in-hospital cardiac arrest is associated with survival to hospital discharge.
Design, Setting, and Participants: Observational cohort study of adult patients who had an in-hospital cardiac arrest from January 2000 through December 2014 included in the Get With The Guidelines-Resuscitation registry, a US-based multicenter registry of in-hospital cardiac arrest. Patients who had an invasive airway in place at the time of cardiac arrest were excluded. Patients intubated at any given minute (from 0-15 minutes) were matched with patients at risk of being intubated within the same minute (ie, still receiving resuscitation) based on a time-dependent propensity score calculated from multiple patient, event, and hospital characteristics.
Exposure: Tracheal intubation during cardiac arrest.
Main Outcomes and Measures: The primary outcome was survival to hospital discharge. Secondary outcomes included return of spontaneous circulation (ROSC) and a good functional outcome. A cerebral performance category score of 1 (mild or no neurological deficit) or 2 (moderate cerebral disability) was considered a good functional outcome.
Results: The propensity-matched cohort was selected from 108 079 adult patients at 668 hospitals. The median age was 69 years (interquartile range, 58-79 years), 45 073 patients (42%) were female, and 24 256 patients (22.4%) survived to hospital discharge. Of 71 615 patients (66.3%) who were intubated within the first 15 minutes, 43 314 (60.5%) were matched to a patient not intubated in the same minute. Survival was lower among patients who were intubated compared with those not intubated: 7052 of 43 314 (16.3%) vs 8407 of 43 314 (19.4%), respectively (risk ratio [RR] = 0.84; 95% CI, 0.81-0.87; P < .001). The proportion of patients with ROSC was lower among intubated patients than those not intubated: 25 022 of 43 311 (57.8%) vs 25 685 of 43 310 (59.3%), respectively (RR = 0.97; 95% CI, 0.96-0.99; P < .001). Good functional outcome was also lower among intubated patients than those not intubated: 4439 of 41 868 (10.6%) vs 5672 of 41 733 (13.6%), respectively (RR = 0.78; 95% CI, 0.75-0.81; P < .001). Although differences existed in prespecified subgroup analyses, intubation was not associated with improved outcomes in any subgroup.
Conclusions and Relevance: Among adult patients with in-hospital cardiac arrest, initiation of tracheal intubation within any given minute during the first 15 minutes of resuscitation, compared with no intubation during that minute, was associated with decreased survival to hospital discharge. Although the study design does not eliminate the potential for confounding by indication, these findings do not support early tracheal intubation for adult in-hospital cardiac arrest.
Lars W Andersen, Asger Granfeldt, Clifton W Callaway, Steven M Bradley, Jasmeet Soar, Jerry P Nolan, Tobias Kurth, Michael W Donnino
JAMA: the Journal of the American Medical Association 2017 January 24
Importance: Tracheal intubation is common during adult in-hospital cardiac arrest, but little is known about the association between tracheal intubation and survival in this setting.
Objective: To determine whether tracheal intubation during adult in-hospital cardiac arrest is associated with survival to hospital discharge.
Design, Setting, and Participants: Observational cohort study of adult patients who had an in-hospital cardiac arrest from January 2000 through December 2014 included in the Get With The Guidelines-Resuscitation registry, a US-based multicenter registry of in-hospital cardiac arrest. Patients who had an invasive airway in place at the time of cardiac arrest were excluded. Patients intubated at any given minute (from 0-15 minutes) were matched with patients at risk of being intubated within the same minute (ie, still receiving resuscitation) based on a time-dependent propensity score calculated from multiple patient, event, and hospital characteristics.
Exposure: Tracheal intubation during cardiac arrest.
Main Outcomes and Measures: The primary outcome was survival to hospital discharge. Secondary outcomes included return of spontaneous circulation (ROSC) and a good functional outcome. A cerebral performance category score of 1 (mild or no neurological deficit) or 2 (moderate cerebral disability) was considered a good functional outcome.
Results: The propensity-matched cohort was selected from 108 079 adult patients at 668 hospitals. The median age was 69 years (interquartile range, 58-79 years), 45 073 patients (42%) were female, and 24 256 patients (22.4%) survived to hospital discharge. Of 71 615 patients (66.3%) who were intubated within the first 15 minutes, 43 314 (60.5%) were matched to a patient not intubated in the same minute. Survival was lower among patients who were intubated compared with those not intubated: 7052 of 43 314 (16.3%) vs 8407 of 43 314 (19.4%), respectively (risk ratio [RR] = 0.84; 95% CI, 0.81-0.87; P < .001). The proportion of patients with ROSC was lower among intubated patients than those not intubated: 25 022 of 43 311 (57.8%) vs 25 685 of 43 310 (59.3%), respectively (RR = 0.97; 95% CI, 0.96-0.99; P < .001). Good functional outcome was also lower among intubated patients than those not intubated: 4439 of 41 868 (10.6%) vs 5672 of 41 733 (13.6%), respectively (RR = 0.78; 95% CI, 0.75-0.81; P < .001). Although differences existed in prespecified subgroup analyses, intubation was not associated with improved outcomes in any subgroup.
Conclusions and Relevance: Among adult patients with in-hospital cardiac arrest, initiation of tracheal intubation within any given minute during the first 15 minutes of resuscitation, compared with no intubation during that minute, was associated with decreased survival to hospital discharge. Although the study design does not eliminate the potential for confounding by indication, these findings do not support early tracheal intubation for adult in-hospital cardiac arrest.
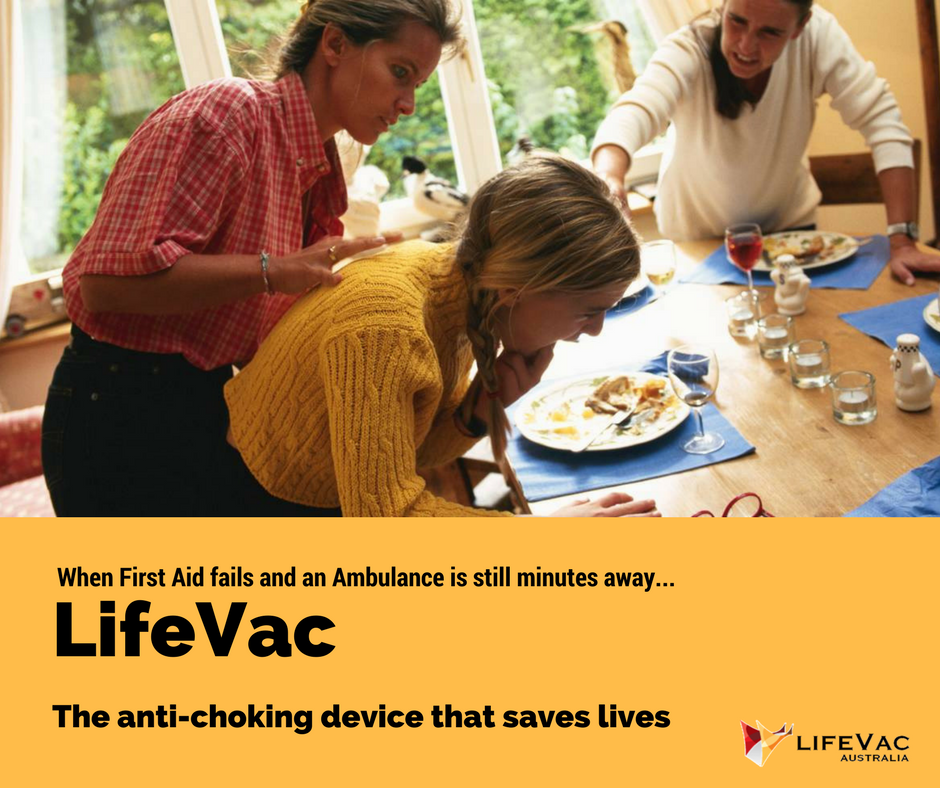
New Emergency Anti-Choking Device - LifeVac now available in Australia
Designed to be used when first aid fails, the LifeVac has already saved 6 lives. The device comes in two configurations. The first for home or facility use that can be wall mounted. The other for storage in existing kits for use by first responders and paramedics. The device can also be used on yourself.
As a comparison, the ARC, one-handed chest thrusts technique for the relief of upper airway obstruction in the conscious adult, rather than abdominal thrusts (used in every country in the world other than AU and NZ) has no relevant clinical evidence, has no clinical trials and has no recorded examples of success in over 15 years of its inception. This is one of the reasons LifeVac saw Australia as a country in need of a device such as the LifeVac.
If we compare the evidence to support LifeVac with the ARC recommendation of one-handed chest thrusts technique:
LifeVac ARC Recommendation
Cadaver Studies Yes No
Manikin Studies Yes No
Used Internationally Yes No
Evidence of Success Yes No
(Note: The studies conducted by LifeVac on our device are available on the website www.lifevac.net.au)
Considering the comparison table above and the level of evidence required to suggest “best practice” it is surprising that this device is not more widespread in Australia over unproven recommendations. Disappointing, but again so predictably when it comes to innovation that trumps their consensus opinion, the ARC refused to allow this new technology to be presented at their recent Spark of Life Conference. Reinforcing again the ARC focus on politics and monopoly control rather than saving lives.
ARAN fully endorses the LifeVac anti-choking device for the removal of upper airway obstruction after the failure of first aid measures. In making this determination, ARAN notes that the device has more evidence of efficacy than the ARC "one-handed chest thrusts technique", currently recommended by the ARC over abdominal thrusts.
As a comparison, the ARC, one-handed chest thrusts technique for the relief of upper airway obstruction in the conscious adult, rather than abdominal thrusts (used in every country in the world other than AU and NZ) has no relevant clinical evidence, has no clinical trials and has no recorded examples of success in over 15 years of its inception. This is one of the reasons LifeVac saw Australia as a country in need of a device such as the LifeVac.
If we compare the evidence to support LifeVac with the ARC recommendation of one-handed chest thrusts technique:
LifeVac ARC Recommendation
Cadaver Studies Yes No
Manikin Studies Yes No
Used Internationally Yes No
Evidence of Success Yes No
(Note: The studies conducted by LifeVac on our device are available on the website www.lifevac.net.au)
Considering the comparison table above and the level of evidence required to suggest “best practice” it is surprising that this device is not more widespread in Australia over unproven recommendations. Disappointing, but again so predictably when it comes to innovation that trumps their consensus opinion, the ARC refused to allow this new technology to be presented at their recent Spark of Life Conference. Reinforcing again the ARC focus on politics and monopoly control rather than saving lives.
ARAN fully endorses the LifeVac anti-choking device for the removal of upper airway obstruction after the failure of first aid measures. In making this determination, ARAN notes that the device has more evidence of efficacy than the ARC "one-handed chest thrusts technique", currently recommended by the ARC over abdominal thrusts.
36 US States now require high school students to learn CPR prior to graduation. 0 Australian states require students to learn CPR prior to graduation (FAIL)
South Dakota has become the latest US state that requires high school students to learn CPR (including defibrillation) prior to graduation
http://news.heart.org/south-dakota-becomes-36th-state-to-require-cpr-to-graduate-high-school/
South Dakota has become the latest US state that requires high school students to learn CPR (including defibrillation) prior to graduation
http://news.heart.org/south-dakota-becomes-36th-state-to-require-cpr-to-graduate-high-school/
ARAN released draft of new ASHPA - Universal BLS Emergency Guideine
For years the DRSABCD (with minor tweaks) has been the standard advice when approaching any BLS emergency. However since its inception there has also been a sense amongst those who have had to use or teach this guideline that it is not a good fit for emergencies that are not a collapse and provides no overall guidance for managing any other type of incident. The other issue is that even if used in a collapse the DRSABCD provides guidance about providing care to a hypoxic arrest in an otherwise healthy casualty - a scenario that really happens. We have found at least 10 advantages of the ASHPA Guideline over the DRSABCD and you may find more. The ASHPA also builds on the 2 critical questions in BLS (consciousness/ unconsciousness and if breathing is normal) to guide the next steps, regardless of the emergency.
Check it out in our "Flowcharts" section
Check it out in our "Flowcharts" section
Compression-to-Ventilation Ratio and Incidence of Rearrest - A Secondary Analysis of the ROC CCC Trial.
A new look at continuous compressions vs. the 30:2 ratio and if CCC produces better, worse or comparable rates of rearrest post ROSC.
NEW UK Resuscitation Council AED Posters and Signs.
After a national survey of consumers, the UK Resuscitation Council has released new posters and signs for AEDs. The content, although not clinically accurate was the consensus among consumers of the easiest messages about AED to understand. ARAN has change the emergency number to 000 and the material is now available for download in pdf.
New cheaper competitor to Epipen coming later this year.
This photo provided by Adamis Pharmaceuticals Corp. shows the Symjepi syringe, prefilled with the hormone epinephrine, which helps stop life-threatening allergic reactions from insect stings and bites or eating foods such as nuts and eggs. On Thursday, June 15, 2017, the Food and Drug Administration approved the Adamis Pharmaceuticals Corp. product, which is expected to go on sale later in 2017. (Audacity Health/Courtesy of Adamis Pharmaceuticals Corp. via AP)
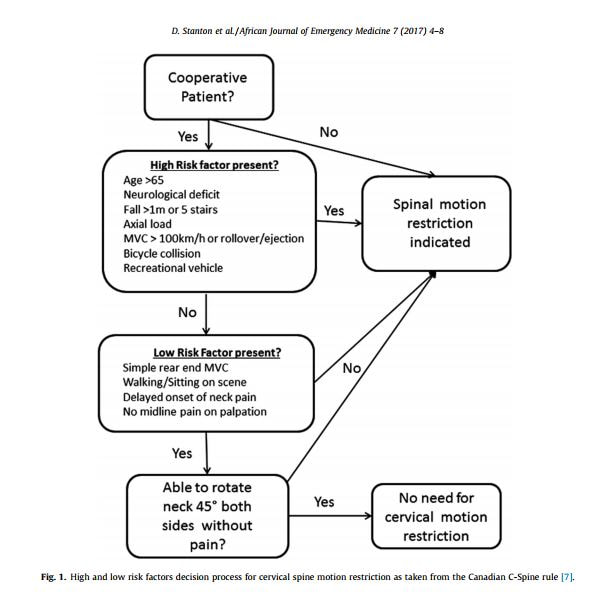
African Journal of Emergency Medicine
Cervical collars and immobilisation: A South African best practice recommendation
Quality of bystander cardiopulmonary resuscitation during real-life out-of-hospital cardiac arrest. Tore Gyllenborg, Asger Granfeldt, Freddy Lippert, Ingunn Skogstad Riddervold, Fredrik Folke
Resuscitation 2017 September 10
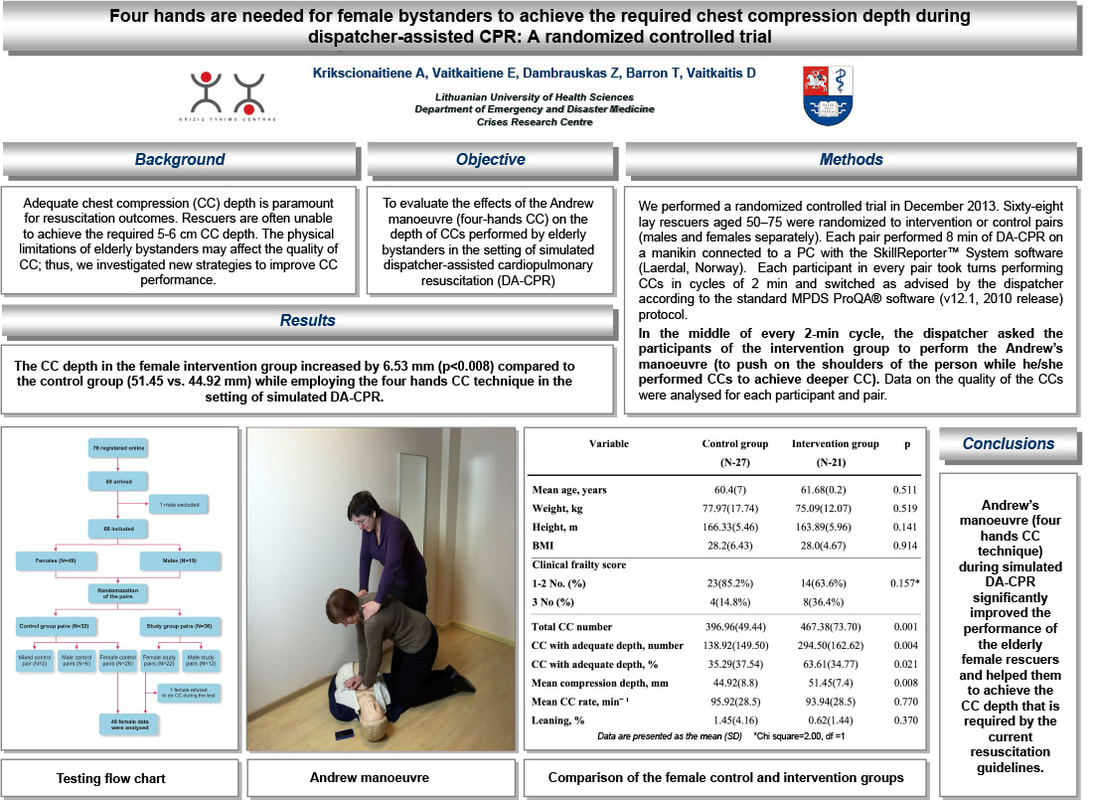
This study conducted in the Capital Region, Denmark, (2012-2016) the initial 10 minutes of CPR data were analysed for compression rate, depth, fraction and compressions delivered for each minute of CPR. Data are presented as median [25th;75th percentile]. The study included 136 cases. Bystander median compression rate was 101min (-1) [94;113], compression depth was 48mm [3.9;5.8] and compressions per minute were 62 [48;73]. Of all cases, the median compression rate was 100-120min (-1) in 42%, compression depth was 50 -60mm (i.e in compliance with current recommendations) in 26%, compression fraction≥60% in 51% and compressions delivered per minute exceeded 60 in 54%. In a minute-to-minute analysis, the found no evidence of deterioration in CPR quality over time. The median peri-shock pause was 27s [23;31] and the pre-shock pause was 19s [17;22].
CONCLUSION: The median CPR performed by bystanders using AEDs with audio-feedback in OHCA was within guideline recommendations without deterioration over time. Compression depth had poorer quality compared with other parameters. To improve bystander CPR quality, focus should be on proper compression depth and minimizing pauses.
ARAN Comment: This data (although from an AED using a accellerometer feedback) reinforces the importance of compression depth (as only 42% were in the recommended range). Unfortunately, most training manikins (that are under no standard), do not realistically simulated the force pressure required for compressions on a typical cardiac arrest victim. Two recommendations would be: 1. A standard for resuscitation manikins and 2. Training emphasis on the minimisation of pauses e.g. high performance cpr.
CONCLUSION: The median CPR performed by bystanders using AEDs with audio-feedback in OHCA was within guideline recommendations without deterioration over time. Compression depth had poorer quality compared with other parameters. To improve bystander CPR quality, focus should be on proper compression depth and minimizing pauses.
ARAN Comment: This data (although from an AED using a accellerometer feedback) reinforces the importance of compression depth (as only 42% were in the recommended range). Unfortunately, most training manikins (that are under no standard), do not realistically simulated the force pressure required for compressions on a typical cardiac arrest victim. Two recommendations would be: 1. A standard for resuscitation manikins and 2. Training emphasis on the minimisation of pauses e.g. high performance cpr.
Frequency and influencing factors of cardiopulmonary resuscitation-related injuries during implementation of the American Heart Association 2010 Guidelines: a retrospective study based on autopsy and postmortem computed tomography. Rutsuko Yamaguchi, Yohsuke Makino, Fumiko Chiba, Suguru Torimitsu, Daisuke Yajima, Go Inokuchi, Ayumi Motomura, Mari Hashimoto, Yumi Hoshioka, Tomohiro Shinozaki, Hirotaro Iwase
International Journal of Legal Medicine 2017 September 13
The study conducted between January 2012 to December 2014 tried to determine the frequency of cardiopulmonary resuscitation (CPR)-related injuries and factors involved in their occurrence, data based on forensic autopsy and postmortem computed tomography (PMCT) during implementation of the 2010 American Heart Association Guidelines for CPR were studied.
RESULTS: In total, 180 consecutive cases were analyzed. Rib fractures and sternal fractures were most frequent (overall frequency, 66.1 and 52.8%, respectively), followed by heart injuries (12.8%) and abdominal visceral injuries (2.2%). Urgently life-threatening injuries were rare (2.8%). Older age was an independent risk factor for rib fracture [adjusted odds ratio (AOR), 1.06; 95% confidence interval (CI), 1.04-1.08; p < 0.001], ≥ 3 rib fractures (AOR, 1.06; 95% CI, 1.02-1.09; p = 0.002), and sternal fracture (AOR, 1.03; 95% CI, 1.01-1.05; p < 0.001). Female sex was significantly associated with sternal fracture (AOR, 2.08; 95% CI, 1.02-4.25; p = 0.04). Chest compression only by laypersons was inversely associated with rib and sternal fractures. Body mass index and in-hospital cardiac arrest were not significantly associated with any complications. The frequency of thoracic skeletal injuries was similar to that in recent autopsy-based studies.
ARAN Comment: The significant findings of low numbers of injuries is consistent with other findings. The association of age and musculo-skeletal injuries is self evident. The significant finding was that chest compression only CPR by bystanders was inversely associated with complications like rib and sternal fractures. This is further evidence that compression only CPR is a superior method for public BLS training, particularly in the first 6-8 minutes in SCA.
RESULTS: In total, 180 consecutive cases were analyzed. Rib fractures and sternal fractures were most frequent (overall frequency, 66.1 and 52.8%, respectively), followed by heart injuries (12.8%) and abdominal visceral injuries (2.2%). Urgently life-threatening injuries were rare (2.8%). Older age was an independent risk factor for rib fracture [adjusted odds ratio (AOR), 1.06; 95% confidence interval (CI), 1.04-1.08; p < 0.001], ≥ 3 rib fractures (AOR, 1.06; 95% CI, 1.02-1.09; p = 0.002), and sternal fracture (AOR, 1.03; 95% CI, 1.01-1.05; p < 0.001). Female sex was significantly associated with sternal fracture (AOR, 2.08; 95% CI, 1.02-4.25; p = 0.04). Chest compression only by laypersons was inversely associated with rib and sternal fractures. Body mass index and in-hospital cardiac arrest were not significantly associated with any complications. The frequency of thoracic skeletal injuries was similar to that in recent autopsy-based studies.
ARAN Comment: The significant findings of low numbers of injuries is consistent with other findings. The association of age and musculo-skeletal injuries is self evident. The significant finding was that chest compression only CPR by bystanders was inversely associated with complications like rib and sternal fractures. This is further evidence that compression only CPR is a superior method for public BLS training, particularly in the first 6-8 minutes in SCA.
Association of Public Health Initiatives With Outcomes for Out-of-Hospital Cardiac Arrest at Home and in Public Locations
Christopher B Fordyce, Carolina M Hansen, Kristian Kragholm, Matthew E Dupre, James G Jollis, Mayme L Roettig, Lance B Becker, Steen M Hansen, Tomoya T Hinohara, Claire C Corbett, Lisa Monk, R Darrell Nelson, David A Pearson, Clark Tyson, Sean van Diepen, Monique L Anderson, Bryan McNally, Christopher B Granger
JAMA Cardiology 2017 October 4
Importance: Little is known about the influence of comprehensive public health initiatives according to out-of-hospital cardiac arrest (OHCA) location, particularly at home, where resuscitation efforts and outcomes have historically been poor.
Objective: To describe temporal trends in bystander cardiopulmonary resuscitation (CPR) and first-responder defibrillation for OHCAs stratified by home vs public location and their association with survival and neurological outcomes.
Design, Setting, and Participants: This observational study reviewed 8269 patients with OHCAs (5602 [67.7%] at home and 2667 [32.3%] in public) for whom resuscitation was attempted using data from the Cardiac Arrest Registry to Enhance Survival (CARES) from January 1, 2010, through December 31, 2014. The setting was 16 counties in North Carolina.
Exposures: Patients were stratified by home vs public OHCA. Public health initiatives to improve bystander and first-responder interventions included training members of the general population in CPR and in the use of automated external defibrillators, teaching first responders about team-based CPR (eg, automated external defibrillator use and high-performance CPR), and instructing dispatch centres on recognition of cardiac arrest.
Main Outcomes and Measures: Association of resuscitation efforts with survival and neurological outcomes from 2010 through 2014.
Results: Among home OHCA patients (n = 5602), the median age was 64 years, and 62.2% were male; among public OHCA patients (n = 2667), the median age was 68 years, and 61.5% were male. After comprehensive public health initiatives, the proportion of patients receiving bystander CPR increased at home (from 28.3% [275 of 973] to 41.3% [498 of 1206], P < .001) and in public (from 61.0% [275 of 451] to 70.5% [424 of 601], P = .01), while first-responder defibrillation increased at home (from 42.2% [132 of 313] to 50.8% [212 of 417], P = .02) but not significantly in public (from 33.1% [58 of 175] to 37.8% [93 of 246], P = .17). Survival to discharge improved for arrests at home (from 5.7% [60 of 1057] to 8.1% [100 of 1238], P = .047) and in public (from 10.8% [50 of 464] to 16.2% [98 of 604], P = .04). Compared with emergency medical services-initiated CPR and resuscitation, patients with home OHCA were significantly more likely to survive to hospital discharge if they received bystander-initiated CPR and first-responder defibrillation (odds ratio, 1.55; 95% CI, 1.01-2.38). Patients with arrests in public were most likely to survive if they received both bystander-initiated CPR and defibrillation (odds ratio, 4.33; 95% CI, 2.11-8.87).
Conclusions and Relevance: After coordinated and comprehensive public health initiatives, more patients received bystander CPR and first-responder defibrillation at home and in public, which was associated with improved survival.
ARAN Comment:: Whilst the outcomes of this research are predictable and obvious we in Australia see not State or Federal Government interest in OHCA through public education and initiative. The NHS in the UK funds defibrillators in communities. In Australia the emphasis is on Ambulance and ED's saving lives in OHCA., however the pre-Ambulance phase is where we can see the real improvements. to our appalling survival rate. (5-6% to hospital discharge in Adults). i.e. only 1,980 lives out of 33,500 (and up to 75% are savable). Road fatalities only account for 1.,155 deaths a year and have been relatively static of the past 7 years (regardless of the heavy policing of marginal speed infringements, speed cameras, television advertising, double demerits and all the public advertising . Road safety campaigns and processes cost over $500 million dollars per year in Australia i.e nearly 1/2 a million dollars for every death. ARAN has written to both State and Federal Health Ministers concerning improving the national situation, however it has been made very clear that there is no appetite or interest in OHCA in Australian government.
Continuous chest compression versus interrupted chest compression for cardiopulmonary resuscitation of non-asphyxial out-of-hospital cardiac arrest
Lei Zhan, Li J Yang, Yu Huang, Qing He, Guan J Liu
Cochrane Database of Systematic Reviews 2017 March 27, 3: CD010134
BACKGROUND: Out-of-hospital cardiac arrest (OHCA) is a major cause of death worldwide. Cardiac arrest can be subdivided into asphyxial and non asphyxial etiologies. An asphyxia arrest is caused by lack of oxygen in the blood and occurs in drowning and choking victims and in other circumstances. A non asphyxial arrest is usually a loss of functioning cardiac electrical activity. Cardiopulmonary resuscitation (CPR) is a well-established treatment for cardiac arrest. Conventional CPR includes both chest compressions and 'rescue breathing' such as mouth-to-mouth breathing. Rescue breathing is delivered between chest compressions using a fixed ratio, such as two breaths to 30 compressions or can be delivered asynchronously without interrupting chest compression. Studies show that applying continuous chest compressions is critical for survival and interrupting them for rescue breathing might increase risk of death. Continuous chest compression CPR may be performed with or without rescue breathing.
OBJECTIVES: To assess the effects of continuous chest compression CPR (with or without rescue breathing) versus conventional CPR plus rescue breathing (interrupted chest compression with pauses for breaths) of non-asphyxial OHCA.
SEARCH METHODS: We searched the Cochrane Central Register of Controlled Trials (CENTRAL; Issue 1 2017); MEDLINE (Ovid) (from 1985 to February 2017); Embase (1985 to February 2017); Web of Science (1985 to February 2017). We searched ongoing trials databases including controlledtrials.com and clinicaltrials.gov. We did not impose any language or publication restrictions.
SELECTION CRITERIA: We included randomized and quasi-randomized studies in adults and children suffering non-asphyxial OHCA due to any cause. Studies compared the effects of continuous chest compression CPR (with or without rescue breathing) with interrupted CPR plus rescue breathing provided by rescuers (bystanders or professional CPR providers).
DATA COLLECTION AND ANALYSIS: Two authors extracted the data and summarized the effects as risk ratios (RRs), adjusted risk differences (ARDs) or mean differences (MDs). We assessed the quality of evidence using GRADE.
MAIN RESULTS: We included three randomized controlled trials (RCTs) and one cluster-RCT (with a total of 26,742 participants analysed). We identified one ongoing study. While predominantly adult patients, one study included children. Untrained bystander-administered CPR. Three studies assessed CPR provided by untrained bystanders in urban areas of the USA, Sweden and the UK. Bystanders administered CPR under telephone instruction from emergency services. There was an unclear risk of selection bias in two trials and low risk of detection, attrition, and reporting bias in all three trials. Survival outcomes were unlikely to be affected by the unblinded design of the studies.We found high-quality evidence that continuous chest compression CPR without rescue breathing improved participants' survival to hospital discharge compared with interrupted chest compression with pauses for rescue breathing (ratio 15:2) by 2.4% (14% versus 11.6%; RR 1.21, 95% confidence interval (CI) 1.01 to 1.46; 3 studies, 3031 participants).One trial reported survival to hospital admission, but the number of participants was too low to be certain about the effects of the different treatment strategies on survival to admission(RR 1.18, 95% CI 0.94 to 1.48; 1 study, 520 participants; moderate-quality evidence).There were no data available for survival at one year, quality of life, return of spontaneous circulation or adverse effects.There was insufficient evidence to determine the effect of the different strategies on neurological outcomes at hospital discharge (RR 1.25, 95% CI 0.94 to 1.66; 1 study, 1286 participants; moderate-quality evidence). The proportion of participants categorized as having good or moderate cerebral performance was 11% following treatment with interrupted chest compression plus rescue breathing compared with 10% to 18% for those treated with continuous chest compression CPR without rescue breathing. CPR administered by a trained professional In one trial that assessed OHCA CPR administered by emergency medical service professionals (EMS) 23,711 participants received either continuous chest compression CPR (100/minute) with asynchronous rescue breathing (10/minute) or interrupted chest compression with pauses for rescue breathing (ratio 30:2). The study was at low risk of bias overall.After OHCA, risk of survival to hospital discharge is probably slightly lower for continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (9.0% versus 9.7%) with an adjusted risk difference (ARD) of -0.7%; 95% CI (-1.5% to 0.1%); moderate-quality evidence.There is high-quality evidence that survival to hospital admission is 1.3% lower with continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (24.6% versus 25.9%; ARD -1.3% 95% CI (-2.4% to -0.2%)).Survival at one year and quality of life were not reported.Return of spontaneous circulation is likely to be slightly lower in people treated with continuous chest compression CPR plus asynchronous rescue breathing (24.2% versus 25.3%; -1.1% (95% CI -2.4 to 0.1)), high-quality evidence.There is high-quality evidence of little or no difference in neurological outcome at discharge between these two interventions (7.0% versus 7.7%; ARD -0.6% (95% CI -1.4 to 0.1).Rates of adverse events were 54.4% in those treated with continuous chest compressions plus asynchronous rescue breathing versus 55.4% in people treated with interrupted chest compression plus rescue breathing compared with the ARD being -1% (-2.3 to 0.4), moderate-quality evidence).
AUTHORS' CONCLUSIONS: Following OHCA, we have found that bystander-administered chest compression-only CPR, supported by telephone instruction, increases the proportion of people who survive to hospital discharge compared with conventional interrupted chest compression CPR plus rescue breathing. Some uncertainty remains about how well neurological function is preserved in this population and there is no information available regarding adverse effects.When CPR was performed by EMS providers, continuous chest compressions plus asynchronous rescue breathing did not result in higher rates for survival to hospital discharge compared to interrupted chest compression plus rescue breathing. The results indicate slightly lower rates of survival to admission or discharge, favourable neurological outcome and return of spontaneous circulation observed following continuous chest compression. Adverse effects are probably slightly lower with continuous chest compression.Increased availability of automated external defibrillators (AEDs), and AED use in CPR need to be examined, and also whether continuous chest compression CPR is appropriate for paediatric cardiac arrest.
ARAN Comment: The study reinforces the benefits of continuous compressions over interrupted compressions, however as with most research does not differentiate between protected vs. unprotected airways and bystander vs. professional intervention and the timing of the onset of different strategies e.g. only on paramedic arrival, from the witnessed event and by whom. These confounders tend to muddy the importance of any findings. The results of the conflation of these variables is often interpreted as inconclusive evidence on which to base change. The significant improvement of cerebral function of those treated with continuous compressions by professionals (18%) over (11%) with current interrupted compressions is an important finding. By inference, the other factor here is that these patients (as they were treated by professionals) would have had a protected airway and not hyperventilated. Again a distinction in management and rescuer would be helpful and probably show a much clearer distinction for change to current recommendations (especially in Australia). The other confounder is that the bystander ability to discern the aetiology of the arrest. The conclusion is once again clear, compression only CPR for bystanders, prior to paramedic arrival leads to better outcomes, particularly in SCA. It is astounding that we have known this since at least 2010 but in Australia we (not all just those looking to for guidelines) are still holding on to an ideology that most arrest are hypoxic in nature and only happen to healthy victims.
Lei Zhan, Li J Yang, Yu Huang, Qing He, Guan J Liu
Cochrane Database of Systematic Reviews 2017 March 27, 3: CD010134
BACKGROUND: Out-of-hospital cardiac arrest (OHCA) is a major cause of death worldwide. Cardiac arrest can be subdivided into asphyxial and non asphyxial etiologies. An asphyxia arrest is caused by lack of oxygen in the blood and occurs in drowning and choking victims and in other circumstances. A non asphyxial arrest is usually a loss of functioning cardiac electrical activity. Cardiopulmonary resuscitation (CPR) is a well-established treatment for cardiac arrest. Conventional CPR includes both chest compressions and 'rescue breathing' such as mouth-to-mouth breathing. Rescue breathing is delivered between chest compressions using a fixed ratio, such as two breaths to 30 compressions or can be delivered asynchronously without interrupting chest compression. Studies show that applying continuous chest compressions is critical for survival and interrupting them for rescue breathing might increase risk of death. Continuous chest compression CPR may be performed with or without rescue breathing.
OBJECTIVES: To assess the effects of continuous chest compression CPR (with or without rescue breathing) versus conventional CPR plus rescue breathing (interrupted chest compression with pauses for breaths) of non-asphyxial OHCA.
SEARCH METHODS: We searched the Cochrane Central Register of Controlled Trials (CENTRAL; Issue 1 2017); MEDLINE (Ovid) (from 1985 to February 2017); Embase (1985 to February 2017); Web of Science (1985 to February 2017). We searched ongoing trials databases including controlledtrials.com and clinicaltrials.gov. We did not impose any language or publication restrictions.
SELECTION CRITERIA: We included randomized and quasi-randomized studies in adults and children suffering non-asphyxial OHCA due to any cause. Studies compared the effects of continuous chest compression CPR (with or without rescue breathing) with interrupted CPR plus rescue breathing provided by rescuers (bystanders or professional CPR providers).
DATA COLLECTION AND ANALYSIS: Two authors extracted the data and summarized the effects as risk ratios (RRs), adjusted risk differences (ARDs) or mean differences (MDs). We assessed the quality of evidence using GRADE.
MAIN RESULTS: We included three randomized controlled trials (RCTs) and one cluster-RCT (with a total of 26,742 participants analysed). We identified one ongoing study. While predominantly adult patients, one study included children. Untrained bystander-administered CPR. Three studies assessed CPR provided by untrained bystanders in urban areas of the USA, Sweden and the UK. Bystanders administered CPR under telephone instruction from emergency services. There was an unclear risk of selection bias in two trials and low risk of detection, attrition, and reporting bias in all three trials. Survival outcomes were unlikely to be affected by the unblinded design of the studies.We found high-quality evidence that continuous chest compression CPR without rescue breathing improved participants' survival to hospital discharge compared with interrupted chest compression with pauses for rescue breathing (ratio 15:2) by 2.4% (14% versus 11.6%; RR 1.21, 95% confidence interval (CI) 1.01 to 1.46; 3 studies, 3031 participants).One trial reported survival to hospital admission, but the number of participants was too low to be certain about the effects of the different treatment strategies on survival to admission(RR 1.18, 95% CI 0.94 to 1.48; 1 study, 520 participants; moderate-quality evidence).There were no data available for survival at one year, quality of life, return of spontaneous circulation or adverse effects.There was insufficient evidence to determine the effect of the different strategies on neurological outcomes at hospital discharge (RR 1.25, 95% CI 0.94 to 1.66; 1 study, 1286 participants; moderate-quality evidence). The proportion of participants categorized as having good or moderate cerebral performance was 11% following treatment with interrupted chest compression plus rescue breathing compared with 10% to 18% for those treated with continuous chest compression CPR without rescue breathing. CPR administered by a trained professional In one trial that assessed OHCA CPR administered by emergency medical service professionals (EMS) 23,711 participants received either continuous chest compression CPR (100/minute) with asynchronous rescue breathing (10/minute) or interrupted chest compression with pauses for rescue breathing (ratio 30:2). The study was at low risk of bias overall.After OHCA, risk of survival to hospital discharge is probably slightly lower for continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (9.0% versus 9.7%) with an adjusted risk difference (ARD) of -0.7%; 95% CI (-1.5% to 0.1%); moderate-quality evidence.There is high-quality evidence that survival to hospital admission is 1.3% lower with continuous chest compression CPR with asynchronous rescue breathing compared with interrupted chest compression plus rescue breathing (24.6% versus 25.9%; ARD -1.3% 95% CI (-2.4% to -0.2%)).Survival at one year and quality of life were not reported.Return of spontaneous circulation is likely to be slightly lower in people treated with continuous chest compression CPR plus asynchronous rescue breathing (24.2% versus 25.3%; -1.1% (95% CI -2.4 to 0.1)), high-quality evidence.There is high-quality evidence of little or no difference in neurological outcome at discharge between these two interventions (7.0% versus 7.7%; ARD -0.6% (95% CI -1.4 to 0.1).Rates of adverse events were 54.4% in those treated with continuous chest compressions plus asynchronous rescue breathing versus 55.4% in people treated with interrupted chest compression plus rescue breathing compared with the ARD being -1% (-2.3 to 0.4), moderate-quality evidence).
AUTHORS' CONCLUSIONS: Following OHCA, we have found that bystander-administered chest compression-only CPR, supported by telephone instruction, increases the proportion of people who survive to hospital discharge compared with conventional interrupted chest compression CPR plus rescue breathing. Some uncertainty remains about how well neurological function is preserved in this population and there is no information available regarding adverse effects.When CPR was performed by EMS providers, continuous chest compressions plus asynchronous rescue breathing did not result in higher rates for survival to hospital discharge compared to interrupted chest compression plus rescue breathing. The results indicate slightly lower rates of survival to admission or discharge, favourable neurological outcome and return of spontaneous circulation observed following continuous chest compression. Adverse effects are probably slightly lower with continuous chest compression.Increased availability of automated external defibrillators (AEDs), and AED use in CPR need to be examined, and also whether continuous chest compression CPR is appropriate for paediatric cardiac arrest.
ARAN Comment: The study reinforces the benefits of continuous compressions over interrupted compressions, however as with most research does not differentiate between protected vs. unprotected airways and bystander vs. professional intervention and the timing of the onset of different strategies e.g. only on paramedic arrival, from the witnessed event and by whom. These confounders tend to muddy the importance of any findings. The results of the conflation of these variables is often interpreted as inconclusive evidence on which to base change. The significant improvement of cerebral function of those treated with continuous compressions by professionals (18%) over (11%) with current interrupted compressions is an important finding. By inference, the other factor here is that these patients (as they were treated by professionals) would have had a protected airway and not hyperventilated. Again a distinction in management and rescuer would be helpful and probably show a much clearer distinction for change to current recommendations (especially in Australia). The other confounder is that the bystander ability to discern the aetiology of the arrest. The conclusion is once again clear, compression only CPR for bystanders, prior to paramedic arrival leads to better outcomes, particularly in SCA. It is astounding that we have known this since at least 2010 but in Australia we (not all just those looking to for guidelines) are still holding on to an ideology that most arrest are hypoxic in nature and only happen to healthy victims.
Technique for chest compressions in adult CPR
Taufiek K Rajab, Charles N Pozner, Claudius Conrad, Lawrence H Cohn, and Jan D Schmitto
Abstract: Chest compressions have saved the lives of countless patients in cardiac arrest as they generate a small but critical amount of blood flow to the heart and brain. This is achieved by direct cardiac massage as well as a thoracic pump mechanism. In order to optimize blood flow excellent chest compression technique is critical. Thus, the quality of the delivered chest compressions is a pivotal determinant of successful resuscitation. If a patient is found unresponsive without a definite pulse or normal breathing then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions. Contra-indications to starting chest compressions include a valid Do Not Attempt Resuscitation Order. Optimal technique for adult chest compressions includes positioning the patient supine, and pushing hard and fast over the center of the chest with the outstretched arms perpendicular to the patient's chest. The rate should be at least 100 compressions per minute and any interruptions should be minimized to achieve a minimum of 60 actually delivered compressions per minute. Aggressive rotation of compressors prevents decline of chest compression quality due to fatigue. Chest compressions are terminated following return of spontaneous circulation. Unconscious patients with normal breathing are placed in the recovery position. If there is no return of spontaneous circulation, then the decision to terminate chest compressions is based on the clinical judgment that the patient's cardiac arrest is unresponsive to treatment. Finally, it is important that family and patients' loved ones who witness chest compressions be treated with consideration and sensitivity.
Introduction: Chest compressions have saved the lives of countless patients in cardiac arrest since they were first introduced in 1960 [1]. Cardiac arrest is treated with cardiopulmonary resuscitation (CPR) and chest compressions are a basic component of CPR. The quality of the delivered chest compressions is a pivotal determinant of successful resuscitation [2]. In spite of this, studies show that the quality of chest compressions, even if delivered by healthcare professionals, is often suboptimal [2]. Therefore it is important that providers carefully familiarize themselves with this technique.
Indications: Chest compressions are generally indicated for all patients in cardiac arrest. Unlike other medical interventions, chest compressions can be initiated by any healthcare provider without a physician's order. This is based on implied patient consent for emergency treatment [3]. If a patient is found unresponsive without a definite pulse or normal breathing then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions [4]. The risk of serious injury from chest compressions to patients who are not in cardiac arrest is negligible [5], while any delay in starting chest compressions has grave implications for outcome. Due to the importance of starting chest compressions early, pulse and breathing checks were de-emphasized in the most recent CPR guidelines [4]. Thus, healthcare providers should take no longer than 10 seconds to check for a pulse. The carotid or femoral pulses are preferred locations for pulse checks since peripheral arteries can be unreliable.
Contraindications: In certain circumstances it is inappropriate to initiate chest compressions. A valid Do Not Resuscitate (DNR) order that prohibits chest compressions is an absolute contra-indication. DNR orders are considered by the attending physician on the basis of patient autonomy and treatment futility.
The principle of patient autonomy dictates that competent patients have a right to refuse medical treatment [6]. Therefore a DNR order should be documented if patients do not wish to be treated with chest compressions. For patients with impaired decision-making, previous preferences should be taken into account when making decisions regarding DNR.
The principle of treatment futility dictates that healthcare providers are not obliged to provide treatment if this would be futile [6]. Therefore a DNR order should be documented if chest compressions would be unlikely to confer a survival benefit or acceptable quality of life. However, few criteria can reliably predict the futility of starting chest compressions.
If there is any uncertainty regarding DNR status then chest compressions should be started immediately while the uncertainties are addressed. Compressions may subsequently be terminated as soon as a valid DNR order is produced.
Of note, patients with implantable left ventricular assist devices [7-9] or patients with total artificial hearts or biventricular assist devices [10] who suffer cardiac arrest from device failure should be resuscitated using a backup pump (e.g. ECMO [11,12]) if this is available rather than with chest compressions.
The Physiology of Chest Compressions: Chest compressions generate a small but critical amount of blood flow to the heart and brain. This significantly improves the chances of successful resuscitation [13]. However, the precise mechanism of blood flow during chest compressions has been controversial since the 1960s. The two main hypotheses are the external cardiac massage model and the thoracic pump model.
The external cardiac massage model suggests that chest compressions directly compress the heart between the depressed sternum and the thoracic spine [1]. This ejects blood into the systemic and pulmonary circulations while backward flow during decompression is limited by the cardiac valves. The external cardiac massage model is supported by radiographic evidence of direct compression of cardiac structures during chest compressions [14].
The thoracic pump model suggests that chest compressions intermittently increase global intra-thoracic pressure, with equivalent pressures exerted on vena cava, the heart and the aorta [9]. Thus blood is ejected retrograde from the intra-thoracic venous vasculature as well as antegrade from the intra-thoracic arterial vasculature and both arterial as well as venous pressures rise concomitantly. Therefore the presence of an arterial pulse in itself is not a reliable indicator of blood flow. This principle is illustrated by the fact that a ligated artery will continue to pulsate even in the absence of blood flow. However, the compliance of venous capacitance vessels is greater than the compliance of arterial resistance vessels. Therefore a pressure differential between the extra-thoracic arterial and venous sides of the vascular tree is formed. This pressure differential is but a fraction of the arterial pulse pressure, yet it is sufficient to drive some blood flow. The thoracic pump model is supported by arterial and venous pressure tracings demonstrating simultaneous peaks in venous and arterial pressures during chest compressions [15].
In toto, the available evidence suggests that both cardiac massage and the thoracic pump contribute to blood flow during chest compressions. Yet even excellent chest compressions can only generate a fraction of baseline blood flow [16]. Therefore the time during chest compressions contributes to the ongoing ischemic insult to the patient's heart and brain.
The brain is the organ most susceptible to decreased blood flow and suffers irreversible damage within 5 minutes of absent perfusion. The myocardium is the second most susceptible organ, with ROSC directly related to coronary perfusion pressures [17]. Therefore successful resuscitation with neurologically intact survival and ROSC critically depends on maintaining blood flow to the heart and brain via chest compressions.
Technique for Chest Compression: Chest compressions consist of forceful and fast oscillations of the lower half of the sternum [1]. The technique of delivering chest compressions is highly standardized and based on international consensus that is updated in 5-year intervals [4,13,18].
Patient PositioningThe patient in cardiac arrest should be placed in supine position with the rescuer standing beside the patient's bed or kneeling beside the patient's chest [18]. Adjustment of the bed height or standing on a stool allows leveraging the body weight above the waist for mechanical advantage. For optimal transfer of energy during chest compressions the patient should be positioned on a firm surface such as a backboard early in resuscitation efforts. This decreases wasting of compressive force by compression of the soft hospital bed. While re-positioning the patient, interruptions of chest compressions should be minimized and care should be taken to avoid dislodging any lines or tubes [13].
Hand Position and PosturePlace the dominant hand over the center of the patient's chest [19]. This position corresponds to the lower half of the sternum. The heel of the hand is positioned in the midline and aligned with the long axis of the sternum. This focuses the compressive force on the sternum and decreases the chance of rib fractures. Next, place the non-dominant hand on top of the first hand so that both hands are overlapped and parallel. The fingers should be elevated off the patient's ribs to minimize compressive force over the ribs. Also avoid compressive force over the xiphisternum or the upper abdomen to minimize iatrogenic injury.
The previously taught method of first identifying anatomical landmarks and then positioning the hands two centimeters above the xiphoid-sternal notch was found to prolong interruptions of chest compressions without an increase in accuracy [20]. Similarly, the use of the internipple line as a landmark for hand placement was found to be unreliable [21]. Therefore these techniques are no longer part of the international consensus guidelines [4,13,18].
For maximum mechanical advantage keep your arms straight and elbows fully extended. Position your shoulders vertically above the patient's sternum. If the compressive force is not perpendicular to the patient's sternum then the patient will roll and part of the compressive force will be lost.
Compression Rate and InterruptionsThe blood flow generated by chest compressions is a function of the number of chest compressions delivered per minute and the effectiveness of each chest compression. The number of compressions delivered per minute is clearly related to survival [22]. This depends on the rate of compressions and the duration of any interruptions. Chest compressions should be delivered at a rate of at least 100 compressions per minute [4] since chest compression rates below 80/min are associated with decreased ROSC [2]. Any interruptions of chest compressions should be minimized. Legitimate reasons to interrupt chest compressions include the delivery of non-invasive rescue breaths, the need to assess rhythm or ROSC, and defibrillation [18]. Hold compressions when non-invasive rescue breaths are delivered [18]. Once an advanced airway is established there is no need to hold compressions for further breaths. High-quality compressions must also continue while defibrillation pads are applied and the defibrillator is prepared [13]. Aim to minimize interruption of chest compressions during the changeover of rescuers. Including all interruptions the patient should receive at least 60 compressions per minute [13].
Compression Depth, Recoil and Duty CycleCompression depth should be at least 5 cm, since sternal depression of 5 cm and over results in a higher ROSC [18]. No upper limit for compression depth has been established in human studies but experts recommend that sternal depression should not exceed 6 cm [13].
After each compression, allow the chest to recoil completely. Incomplete recoil results in worse hemodynamics, including decreased cardiac perfusion, cerebral perfusion and cardiac output [23]. Complete recoil is achieved by releasing all pressure from the chest and not leaning on the chest during the relaxation phase of the chest compressions [13]. However, avoid lifting the hands off the patient's chest, since this was associated with a reduction in compression depth [24].
The duration of the compression phase as a proportion of the total cycle is termed duty cycle. Although duty cycles ranging between 20% and 50% can result in adequate cardiac and cerebral perfusion [25], a duty cycle of 50% is recommended because it is easy to achieve with practice [4]. Thus the duration of the compression phase should be equivalent to the duration of the decompression phase. If the patient has hemodynamic monitoring via an arterial line then compression rate, compression depth and recoil can be optimized for the individual patient on the basis of this data.
Rotating RescuersThe quality of chest compressions deteriorates over time due to fatigue [26]. Therefore the compressor should be rotated every two minutes [13]. Rotating compressors more frequently than this may have detrimental effects due to interruptions of chest compressions from the practicalities of the changeover [27]. Consider rotating compressors during any intervention associated with appropriate interruptions of chest compressions, for example when defibrillating. Every effort should be made to accomplish the switch in less than five seconds. For this purpose it may be helpful for the compressor performing chest compressions to count out loud [13]. If the rotating compressors can be positioned on either side of the patient, one compressor can be ready and waiting to relieve the working compressor in an instant [4].
Termination of Efforts: Chest compressions are terminated following ROSC and unconscious patients with normal breathing are placed in the recovery position [28]. If there is no ROSC, then the decision to terminate efforts is based on the clinical judgment that the patient's arrest is unresponsive to treatment. This decision should be made by the physician leading the emergency response team after consultation with the members of the team. The factors that are considered include the time to initiate chest compressions, duration of chest compressions, initial arrest rhythm, age, comorbidities and any reversible causes of cardiac arrest such as drug overdose [3]. The duration of cardiac arrest is the most important prognostic factor [29]. In general, chest compressions should be continued at least as long as VF persists. Prolonged chest compressions are less likely to succeed if there is no ROSC within half an hour. However, case reports with exceptional ROSC are well documented and each decision to terminate efforts should be made individually. Any family members and patients' loved ones who witness chest compressions should be treated with consideration and sensitivity.
Complications: Life-threatening complications of chest compressions are extremely rare [24]. Such complications occur less frequently than 1% [30-35]. If hypotension is noted following ROSC then cardiogenic shock and abdominal injury are the most important complications of chest compressions that should be considered [31]. Rib fractures are the most frequent complication, with an incidence of 1/3 at autopsy [30]. However, rib fractures were noted in only 2% of non-arrest patients who received chest compressions from a bystander [5]. Following successful ROSC all patients should be re-evaluated for resuscitation-related injuries [28].
Summary: High quality chest compressions are proven to save lives. If an unresponsive patient has no definite pulse or is not breathing normally then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions. Push hard and fast over the center of the chest. Minimize interruptions of chest compressions and aggressively rotate compressors. Following successful ROSC place the patient in the recovery position and re-evaluate for resuscitation-related injuries. If there is no reasonable chance for ROSC then the decision to terminate efforts should be made by the leader of the emergency response team. Any family members witnessing chest compressions should be treated with sensitivity and respect.
References
ARAN Comment: Although this research was first published in 2011 it is a good example of how in resuscitation recommendations, there is an accepted wisdom around technique, rationale and mechanism that have been perpetuation; not because they are continually validated by emerging evidence but because they are not revisited and/or tested for efficacy, since they are considered by some to be "decided". Examples in this research of this unproven "accepted wisdom" include:
Taufiek K Rajab, Charles N Pozner, Claudius Conrad, Lawrence H Cohn, and Jan D Schmitto
Abstract: Chest compressions have saved the lives of countless patients in cardiac arrest as they generate a small but critical amount of blood flow to the heart and brain. This is achieved by direct cardiac massage as well as a thoracic pump mechanism. In order to optimize blood flow excellent chest compression technique is critical. Thus, the quality of the delivered chest compressions is a pivotal determinant of successful resuscitation. If a patient is found unresponsive without a definite pulse or normal breathing then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions. Contra-indications to starting chest compressions include a valid Do Not Attempt Resuscitation Order. Optimal technique for adult chest compressions includes positioning the patient supine, and pushing hard and fast over the center of the chest with the outstretched arms perpendicular to the patient's chest. The rate should be at least 100 compressions per minute and any interruptions should be minimized to achieve a minimum of 60 actually delivered compressions per minute. Aggressive rotation of compressors prevents decline of chest compression quality due to fatigue. Chest compressions are terminated following return of spontaneous circulation. Unconscious patients with normal breathing are placed in the recovery position. If there is no return of spontaneous circulation, then the decision to terminate chest compressions is based on the clinical judgment that the patient's cardiac arrest is unresponsive to treatment. Finally, it is important that family and patients' loved ones who witness chest compressions be treated with consideration and sensitivity.
Introduction: Chest compressions have saved the lives of countless patients in cardiac arrest since they were first introduced in 1960 [1]. Cardiac arrest is treated with cardiopulmonary resuscitation (CPR) and chest compressions are a basic component of CPR. The quality of the delivered chest compressions is a pivotal determinant of successful resuscitation [2]. In spite of this, studies show that the quality of chest compressions, even if delivered by healthcare professionals, is often suboptimal [2]. Therefore it is important that providers carefully familiarize themselves with this technique.
Indications: Chest compressions are generally indicated for all patients in cardiac arrest. Unlike other medical interventions, chest compressions can be initiated by any healthcare provider without a physician's order. This is based on implied patient consent for emergency treatment [3]. If a patient is found unresponsive without a definite pulse or normal breathing then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions [4]. The risk of serious injury from chest compressions to patients who are not in cardiac arrest is negligible [5], while any delay in starting chest compressions has grave implications for outcome. Due to the importance of starting chest compressions early, pulse and breathing checks were de-emphasized in the most recent CPR guidelines [4]. Thus, healthcare providers should take no longer than 10 seconds to check for a pulse. The carotid or femoral pulses are preferred locations for pulse checks since peripheral arteries can be unreliable.
Contraindications: In certain circumstances it is inappropriate to initiate chest compressions. A valid Do Not Resuscitate (DNR) order that prohibits chest compressions is an absolute contra-indication. DNR orders are considered by the attending physician on the basis of patient autonomy and treatment futility.
The principle of patient autonomy dictates that competent patients have a right to refuse medical treatment [6]. Therefore a DNR order should be documented if patients do not wish to be treated with chest compressions. For patients with impaired decision-making, previous preferences should be taken into account when making decisions regarding DNR.
The principle of treatment futility dictates that healthcare providers are not obliged to provide treatment if this would be futile [6]. Therefore a DNR order should be documented if chest compressions would be unlikely to confer a survival benefit or acceptable quality of life. However, few criteria can reliably predict the futility of starting chest compressions.
If there is any uncertainty regarding DNR status then chest compressions should be started immediately while the uncertainties are addressed. Compressions may subsequently be terminated as soon as a valid DNR order is produced.
Of note, patients with implantable left ventricular assist devices [7-9] or patients with total artificial hearts or biventricular assist devices [10] who suffer cardiac arrest from device failure should be resuscitated using a backup pump (e.g. ECMO [11,12]) if this is available rather than with chest compressions.
The Physiology of Chest Compressions: Chest compressions generate a small but critical amount of blood flow to the heart and brain. This significantly improves the chances of successful resuscitation [13]. However, the precise mechanism of blood flow during chest compressions has been controversial since the 1960s. The two main hypotheses are the external cardiac massage model and the thoracic pump model.
The external cardiac massage model suggests that chest compressions directly compress the heart between the depressed sternum and the thoracic spine [1]. This ejects blood into the systemic and pulmonary circulations while backward flow during decompression is limited by the cardiac valves. The external cardiac massage model is supported by radiographic evidence of direct compression of cardiac structures during chest compressions [14].
The thoracic pump model suggests that chest compressions intermittently increase global intra-thoracic pressure, with equivalent pressures exerted on vena cava, the heart and the aorta [9]. Thus blood is ejected retrograde from the intra-thoracic venous vasculature as well as antegrade from the intra-thoracic arterial vasculature and both arterial as well as venous pressures rise concomitantly. Therefore the presence of an arterial pulse in itself is not a reliable indicator of blood flow. This principle is illustrated by the fact that a ligated artery will continue to pulsate even in the absence of blood flow. However, the compliance of venous capacitance vessels is greater than the compliance of arterial resistance vessels. Therefore a pressure differential between the extra-thoracic arterial and venous sides of the vascular tree is formed. This pressure differential is but a fraction of the arterial pulse pressure, yet it is sufficient to drive some blood flow. The thoracic pump model is supported by arterial and venous pressure tracings demonstrating simultaneous peaks in venous and arterial pressures during chest compressions [15].
In toto, the available evidence suggests that both cardiac massage and the thoracic pump contribute to blood flow during chest compressions. Yet even excellent chest compressions can only generate a fraction of baseline blood flow [16]. Therefore the time during chest compressions contributes to the ongoing ischemic insult to the patient's heart and brain.
The brain is the organ most susceptible to decreased blood flow and suffers irreversible damage within 5 minutes of absent perfusion. The myocardium is the second most susceptible organ, with ROSC directly related to coronary perfusion pressures [17]. Therefore successful resuscitation with neurologically intact survival and ROSC critically depends on maintaining blood flow to the heart and brain via chest compressions.
Technique for Chest Compression: Chest compressions consist of forceful and fast oscillations of the lower half of the sternum [1]. The technique of delivering chest compressions is highly standardized and based on international consensus that is updated in 5-year intervals [4,13,18].
Patient PositioningThe patient in cardiac arrest should be placed in supine position with the rescuer standing beside the patient's bed or kneeling beside the patient's chest [18]. Adjustment of the bed height or standing on a stool allows leveraging the body weight above the waist for mechanical advantage. For optimal transfer of energy during chest compressions the patient should be positioned on a firm surface such as a backboard early in resuscitation efforts. This decreases wasting of compressive force by compression of the soft hospital bed. While re-positioning the patient, interruptions of chest compressions should be minimized and care should be taken to avoid dislodging any lines or tubes [13].
Hand Position and PosturePlace the dominant hand over the center of the patient's chest [19]. This position corresponds to the lower half of the sternum. The heel of the hand is positioned in the midline and aligned with the long axis of the sternum. This focuses the compressive force on the sternum and decreases the chance of rib fractures. Next, place the non-dominant hand on top of the first hand so that both hands are overlapped and parallel. The fingers should be elevated off the patient's ribs to minimize compressive force over the ribs. Also avoid compressive force over the xiphisternum or the upper abdomen to minimize iatrogenic injury.
The previously taught method of first identifying anatomical landmarks and then positioning the hands two centimeters above the xiphoid-sternal notch was found to prolong interruptions of chest compressions without an increase in accuracy [20]. Similarly, the use of the internipple line as a landmark for hand placement was found to be unreliable [21]. Therefore these techniques are no longer part of the international consensus guidelines [4,13,18].
For maximum mechanical advantage keep your arms straight and elbows fully extended. Position your shoulders vertically above the patient's sternum. If the compressive force is not perpendicular to the patient's sternum then the patient will roll and part of the compressive force will be lost.
Compression Rate and InterruptionsThe blood flow generated by chest compressions is a function of the number of chest compressions delivered per minute and the effectiveness of each chest compression. The number of compressions delivered per minute is clearly related to survival [22]. This depends on the rate of compressions and the duration of any interruptions. Chest compressions should be delivered at a rate of at least 100 compressions per minute [4] since chest compression rates below 80/min are associated with decreased ROSC [2]. Any interruptions of chest compressions should be minimized. Legitimate reasons to interrupt chest compressions include the delivery of non-invasive rescue breaths, the need to assess rhythm or ROSC, and defibrillation [18]. Hold compressions when non-invasive rescue breaths are delivered [18]. Once an advanced airway is established there is no need to hold compressions for further breaths. High-quality compressions must also continue while defibrillation pads are applied and the defibrillator is prepared [13]. Aim to minimize interruption of chest compressions during the changeover of rescuers. Including all interruptions the patient should receive at least 60 compressions per minute [13].
Compression Depth, Recoil and Duty CycleCompression depth should be at least 5 cm, since sternal depression of 5 cm and over results in a higher ROSC [18]. No upper limit for compression depth has been established in human studies but experts recommend that sternal depression should not exceed 6 cm [13].
After each compression, allow the chest to recoil completely. Incomplete recoil results in worse hemodynamics, including decreased cardiac perfusion, cerebral perfusion and cardiac output [23]. Complete recoil is achieved by releasing all pressure from the chest and not leaning on the chest during the relaxation phase of the chest compressions [13]. However, avoid lifting the hands off the patient's chest, since this was associated with a reduction in compression depth [24].
The duration of the compression phase as a proportion of the total cycle is termed duty cycle. Although duty cycles ranging between 20% and 50% can result in adequate cardiac and cerebral perfusion [25], a duty cycle of 50% is recommended because it is easy to achieve with practice [4]. Thus the duration of the compression phase should be equivalent to the duration of the decompression phase. If the patient has hemodynamic monitoring via an arterial line then compression rate, compression depth and recoil can be optimized for the individual patient on the basis of this data.
Rotating RescuersThe quality of chest compressions deteriorates over time due to fatigue [26]. Therefore the compressor should be rotated every two minutes [13]. Rotating compressors more frequently than this may have detrimental effects due to interruptions of chest compressions from the practicalities of the changeover [27]. Consider rotating compressors during any intervention associated with appropriate interruptions of chest compressions, for example when defibrillating. Every effort should be made to accomplish the switch in less than five seconds. For this purpose it may be helpful for the compressor performing chest compressions to count out loud [13]. If the rotating compressors can be positioned on either side of the patient, one compressor can be ready and waiting to relieve the working compressor in an instant [4].
Termination of Efforts: Chest compressions are terminated following ROSC and unconscious patients with normal breathing are placed in the recovery position [28]. If there is no ROSC, then the decision to terminate efforts is based on the clinical judgment that the patient's arrest is unresponsive to treatment. This decision should be made by the physician leading the emergency response team after consultation with the members of the team. The factors that are considered include the time to initiate chest compressions, duration of chest compressions, initial arrest rhythm, age, comorbidities and any reversible causes of cardiac arrest such as drug overdose [3]. The duration of cardiac arrest is the most important prognostic factor [29]. In general, chest compressions should be continued at least as long as VF persists. Prolonged chest compressions are less likely to succeed if there is no ROSC within half an hour. However, case reports with exceptional ROSC are well documented and each decision to terminate efforts should be made individually. Any family members and patients' loved ones who witness chest compressions should be treated with consideration and sensitivity.
Complications: Life-threatening complications of chest compressions are extremely rare [24]. Such complications occur less frequently than 1% [30-35]. If hypotension is noted following ROSC then cardiogenic shock and abdominal injury are the most important complications of chest compressions that should be considered [31]. Rib fractures are the most frequent complication, with an incidence of 1/3 at autopsy [30]. However, rib fractures were noted in only 2% of non-arrest patients who received chest compressions from a bystander [5]. Following successful ROSC all patients should be re-evaluated for resuscitation-related injuries [28].
Summary: High quality chest compressions are proven to save lives. If an unresponsive patient has no definite pulse or is not breathing normally then the responder should assume that this patient is in cardiac arrest, activate the emergency response system and immediately start chest compressions. Push hard and fast over the center of the chest. Minimize interruptions of chest compressions and aggressively rotate compressors. Following successful ROSC place the patient in the recovery position and re-evaluate for resuscitation-related injuries. If there is no reasonable chance for ROSC then the decision to terminate efforts should be made by the leader of the emergency response team. Any family members witnessing chest compressions should be treated with sensitivity and respect.
References
- Kouwenhoven W, Jude J, Knickerbocker G. Closed-chest cardiac massage. JAMA. 1960;173:1064–7. doi: 10.1001/jama.1960.03020280004002. [PubMed] [Cross Ref]
- Abella BS. et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–34. doi: 10.1161/01.CIR.0000153811.84257.59. [PubMed] [Cross Ref]
- Morrison LJ. et al. Part 3: ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S665–75.[PubMed]
- Berg RA. et al. Part 5: adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S685–705. [PubMed]
- White L. et al. Dispatcher-assisted cardiopulmonary resuscitation: risks for patients not in cardiac arrest. Circulation. 2010;121(1):91–7. doi: 10.1161/CIRCULATIONAHA.109.872366. [PubMed][Cross Ref]
- Lippert FK. et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 10. The ethics of resuscitation and end-of-life decisions. Resuscitation. 2010;81(10):1445–51. doi: 10.1016/j.resuscitation.2010.08.013. [PubMed] [Cross Ref]
- Mokashi SA, Schmitto JD, Lee LS, Rawn JD, Bolman RM, Shekar PS, Couper GS, Chen FY. Ventricular assist device in patients with prosthetic heart valves. Artif Organs. 2010;34(11):1030–4. doi: 10.1111/j.1525-1594.2010.01102.x. [PubMed] [Cross Ref]
- Schmitto JD, Molitoris U, Haverich A, Strueber M. Implantation of a centrifugal pump as a left ventricular assist device through a novel, minimized approach: Upper hemisternotomy combined with anterolateral thoracotomy. J Thorac Cardiovasc Surg. 2011. in press . [PubMed]
- Mokashi SA, Guan J, Wang D, Tchantchaleishvili V, Brigham M, Lipsitz S, Lee LS, Schmitto JD, Bolman RM, Khademhosseini A, Liao R, Chen FY. Preventing cardiac remodeling: the combination of cell-based therapy and cardiac support therapy preserves left ventricular function in rodent model of myocardial ischemia. J Thorac Cardiovasc Surg. 2010;140(6):1374–80. doi: 10.1016/j.jtcvs.2010.07.070. [PubMed] [Cross Ref]
- Strueber M, Schmitto JD, Kutschka I, Haverich A. Placement of two implantable centrifugal pumps to serve as a total artificial heart after cardiectomy. J Thorac Cardiovasc Surg. 2011. [PubMed]
- Coskun KO, Popov AF, Schmitto JD, Hinz J, Kriebel T, Schoendube FA, Ruschewski W, Tirilomis T. Extracorporeal circulation for rewarming in drowning and near-drowning pediatric patients. Artif Organs. 2010;34(11):1026–30. doi: 10.1111/j.1525-1594.2010.01156.x. [PubMed] [Cross Ref]
- Coskun KO, Coskun ST, Popov AF, Hinz J, El-Arousy M, Schmitto JD, Kececioglu D, Koerfer R. Extracorporeal life support in pediatric cardiac dysfunction. J Cardiothorac Surg. 2010;5:112. doi: 10.1186/1749-8090-5-112. [PMC free article] [PubMed] [Cross Ref]
- Koster RW. et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81(10):1277–92. doi: 10.1016/j.resuscitation.2010.08.009. [PubMed] [Cross Ref]
- Hwang SO. et al. Compression of the left ventricular outflow tract during cardiopulmonary resuscitation. Acad Emerg Med. 2009;16(10):928–33. doi: 10.1111/j.1553-2712.2009.00497.x.[PubMed] [Cross Ref]
- Weale FE, Rothwell-Jackson RL. The efficiency of cardiac massage. Lancet. 1962;1(7237):990–2.[PubMed]
- Delguercio LR. et al. Comparison of blood flow during external and internal cardiac massage in man. Circulation. 1965;31(SUPPL 1):171–80. [PubMed]
- Paradis N. et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA. 1990;263(8):1106–13. doi: 10.1001/jama.1990.03440080084029. [PubMed] [Cross Ref]
- Sayre MR. et al. Part 5: Adult basic life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 Suppl 2):S298–324. [PubMed]
- Kundra P, Dey S, Ravishankar M. Role of dominant hand position during external cardiac compression. Br J Anaesth. 2000;84(4):491–3. [PubMed]
- Handley AJ. Teaching hand placement for chest compression--a simpler technique. Resuscitation. 2002;53(1):29–36. doi: 10.1016/S0300-9572(01)00506-8. [PubMed] [Cross Ref]
- Shin J, Rhee JE, Kim K. Is the inter-nipple line the correct hand position for effective chest compression in adult cardiopulmonary resuscitation? Resuscitation. 2007;75(2):305–10. doi: 10.1016/j.resuscitation.2007.05.003. [PubMed] [Cross Ref]
- Christenson J. et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241–7. doi: 10.1161/CIRCULATIONAHA.109.852202. [PMC free article] [PubMed] [Cross Ref]
- Yannopoulos D. et al. Effects of incomplete chest wall decompression during cardiopulmonary resuscitation on coronary and cerebral perfusion pressures in a porcine model of cardiac arrest. Resuscitation. 2005;64(3):363–72. doi: 10.1016/j.resuscitation.2004.10.009. [PubMed] [Cross Ref]
- Aufderheide TP. et al. Incomplete chest wall decompression: a clinical evaluation of CPR performance by EMS personnel and assessment of alternative manual chest compression-decompression techniques. Resuscitation. 2005;64(3):353–62. doi: 10.1016/j.resuscitation.2004.10.007. [PubMed] [Cross Ref]
- Handley AJ, Handley JA. The relationship between rate of chest compression and compression:relaxation ratio. Resuscitation. 1995;30(3):237–41. doi: 10.1016/0300-9572(95)00892-6. [PubMed] [Cross Ref]
- Hightower D. et al. Decay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26(3):300–3. doi: 10.1016/S0196-0644(95)70076-5. [PubMed] [Cross Ref]
- Manders S, Geijsel FE. Alternating providers during continuous chest compressions for cardiac arrest: every minute or every two minutes? Resuscitation. 2009;80(9):1015–8. doi: 10.1016/j.resuscitation.2009.05.014. [PubMed] [Cross Ref]
- Resuscitation IL 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 2: Adult basic life support. Resuscitation. 2005;67(2-3):187–201. [PubMed]
- Schultz SC. et al. Predicting in-hospital mortality during cardiopulmonary resuscitation. Resuscitation. 1996;33(1):13–7. doi: 10.1016/S0300-9572(96)00986-0. [PubMed] [Cross Ref]
- Krischer JP. et al. Complications of cardiac resuscitation. Chest. 1987;92(2):287–91. doi: 10.1378/chest.92.2.287. [PubMed] [Cross Ref]
- Atcheson SG, Fred HL. Letter: Complications of cardiac resuscitation. Am Heart J. 1975;89(2):263–5. [PubMed]
- Schmitto JD, Rajab TK, Cohn LH. Prevalence and variability of internal mammary graft use in contemporary multivessel coronary artery bypass graft. Curr Opin Cardiol. 2010;25(6):609–12. doi: 10.1097/HCO.0b013e32833f0498. [PubMed] [Cross Ref]
- Schmitto JD, Mokashi SA, Cohn LH. Past, present, and future of minimally invasive mitral valve surgery. J Heart Valve Dis. 2011;20(5):493–8. [PubMed]
- Schmitto JD, Mohr FW, Cohn LH. Minimally invasive aortic valve replacement: how does this perform in high-risk patients? Curr Opin Cardiol. 2011;26(2):118–22. doi: 10.1097/HCO.0b013e328343983a. [PubMed] [Cross Ref]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol. 2010;56(6):455–62. doi: 10.1016/j.jacc.2010.03.053. [PubMed] [Cross Ref]
ARAN Comment: Although this research was first published in 2011 it is a good example of how in resuscitation recommendations, there is an accepted wisdom around technique, rationale and mechanism that have been perpetuation; not because they are continually validated by emerging evidence but because they are not revisited and/or tested for efficacy, since they are considered by some to be "decided". Examples in this research of this unproven "accepted wisdom" include:
- The assumption that the ideal hand position is "parallel and overlapping with the fingers elevated off the rib cage".(as this is suppose to mitigate rib fractures. This technique has no supporting evidence as superior or that rib fractures are reduced but is the default description on every website and in current Australian guidelines. ARAN has in its guidelines alternate techniques that are more effective that this accepted wisdom.
- The landmarks used for compression location, simplified to the "centre of the chest" in this and ILCOR guidelines does lead to issues in some larger children for rescuers with large hands, leading to overlap over the xiphoid process. Palpating the lower border of the sternum and using at least a one finger spacing to hand placement minimises complications. Usually in smaller children and infants the centre of the chest is appropriate. The "delay" mentioned in establishing landmarks is not significant if they result in optimal compressions with decreased complications. The paper also states that the incidence of rib fractures (2%) by bystanders and 1/3 on autopsy overall. This result is contradictory and suggests that paramedics have a rib fracture rate 1500% greater than bystanders. either this indicates that bystander compression are largely ineffective, paramedics are heavy-handed or just providing sufficient depth of compression to generate sufficient inter-thoracic pressure change or: the 2% bystander rate of rib fractures (considering these (who would most likely all have autopsy's) is a distorted figure.
- This early work asserts that a "legitimate" reason for the interruption to compressions would be the application of "rescue breaths". Any reader of ARAN works would be familiar with our distaste for the term "rescue breaths" that imply "mouth to" contact with a casualty using expired air, a technique in most bystander arrests leads to hyperventilation, gastric distension and aspiration. Secondly, although this is a 2011 paper, the legitimacy of interrupted CPR in this paper is still championed by the ARC in Australia, for all arrests. The paper is held up with more reverence than other contemporary evidence that continuous compressions are superior.
- The paper does not recognise that there is a significant section of the community who cannot use the kneeling compression technique (let alone effective ventilations, if required). This could be due to age, low body mass, being frail, disability, injury or a medical condition like arthritis, knee or hip replacement or chronic back injury. ARAN has promoted for a number of years the teaching of an alternate technique (using the foot) called "pedal compressions" and this is described on our website. This technique has been used in actual cardiac arrests with outcomes similar to "traditional" methods. Some years ago ARAN sent a paper regarding pedal compression to the ARC for consideration, however to date there has not even been an acknowledgement of the correspondence let alone any evidence of a genuine consideration of this life saving technique. It reinforces the that when the ARC say:
ARAN goes it alone to change the regulations around defibrillators (AEDs).
Together with a few proactive and progressive organisations, ARAN has led a formal submission to the Australian Building Codes Board, suggesting revisions to the 2019 National Construction Code (NCC) and the Building and Construction Code (BCC) to include mandatory provisions of AEDs in buildings to comply with certification.
ARAN believes that this initiative is the best way to reach the density and spread of defibrillators required to show significant improvements in out of hospital cardiac arrest. While over 33,500 people in Australia suffer a sudden cardiac arrest, only 5-6% survive to discharge from hospital. The significant change is what happens in the pre-ambulance period and the most important element in survival is early defibrillation (< 3 mins). The only way to achieve this is to have Public Access Defibrillators as accessible as fire extinguishers and a consistent requirement rather than optional extra. Changes to the building codes mean the certification of certain types of buildings (including change of purpose) for a specified purpose must have AED's available and installed to a standard, including spacing, housing and maintenance.
Currently there are no regulations, laws, legislation, WHS codes or standards that make AEDs a requirement. Australia is reliant on voluntary industry codes and the good will of businesses, organisations and individuals to reach appropriate AED numbers...but this will never result in effective coverage.
Significantly and disappointingly, the ARC where not supportive of this initiative. It is clear that this is due to political ideology rather than merit. History tells us that the modus operandi of the ARC is not to support any initiative originating from outside their organisation but then vigorously attack any proposal once it enters the public comment phase to make their influence felt. Another example of letting down the Australian public with its hubris.
ARAN believes that this initiative is the best way to reach the density and spread of defibrillators required to show significant improvements in out of hospital cardiac arrest. While over 33,500 people in Australia suffer a sudden cardiac arrest, only 5-6% survive to discharge from hospital. The significant change is what happens in the pre-ambulance period and the most important element in survival is early defibrillation (< 3 mins). The only way to achieve this is to have Public Access Defibrillators as accessible as fire extinguishers and a consistent requirement rather than optional extra. Changes to the building codes mean the certification of certain types of buildings (including change of purpose) for a specified purpose must have AED's available and installed to a standard, including spacing, housing and maintenance.
Currently there are no regulations, laws, legislation, WHS codes or standards that make AEDs a requirement. Australia is reliant on voluntary industry codes and the good will of businesses, organisations and individuals to reach appropriate AED numbers...but this will never result in effective coverage.
Significantly and disappointingly, the ARC where not supportive of this initiative. It is clear that this is due to political ideology rather than merit. History tells us that the modus operandi of the ARC is not to support any initiative originating from outside their organisation but then vigorously attack any proposal once it enters the public comment phase to make their influence felt. Another example of letting down the Australian public with its hubris.
Heroic Heimlich! Off-duty New Jersey police officer captured on video saving choking man's life in front of his son
An off-duty New Jersey police officer has been lauded as a 'hero' after he quickly acted to save a man from choking at a restaurant. New Jersey State Trooper Dennis Palaia was with his son watching a football game on Sunday at a Buffalo Wild Wings branch in Rockaway Township, New Jersey when he noticed a distressed man sitting nearby, according to police.
Palaia immediately rushed to the dining man, who was showing signs of difficulty breathing. Recognizing that the man was choking, he immediately began the Heimlich Maneuver,' police said.
After four abdominal thrusts, the off-duty police officer was able to clear the choking man's airway.
Police said that the man was then able to resume breathing and his skin tone - which had changed during the traumatic incident - had returned to its natural colour.
The so-far unnamed victim expressed his eternal gratitude to Palaia for saving his life. Apart from a sore throat and some aching ribs, police reported that the man has since made a full recovery.
By Julie Steigerwald For Dailymail.com
- New Jersey State Trooper Dennis Palaia was with his son watching a football game when he noticed a nearby diner exhibiting signs of distress
- Surveillance footage captured tense moments as police officer performs life-saving first aid manoeuvre to clear the choking man's airway
- Unnamed victim expressed his eternal gratitude to the officer for saving his life
- Palaia 'undoubtedly prevented a tragedy,' police state in praise as hundreds of social media users laud trooper for his quick, life-saving action
An off-duty New Jersey police officer has been lauded as a 'hero' after he quickly acted to save a man from choking at a restaurant. New Jersey State Trooper Dennis Palaia was with his son watching a football game on Sunday at a Buffalo Wild Wings branch in Rockaway Township, New Jersey when he noticed a distressed man sitting nearby, according to police.
Palaia immediately rushed to the dining man, who was showing signs of difficulty breathing. Recognizing that the man was choking, he immediately began the Heimlich Maneuver,' police said.
After four abdominal thrusts, the off-duty police officer was able to clear the choking man's airway.
Police said that the man was then able to resume breathing and his skin tone - which had changed during the traumatic incident - had returned to its natural colour.
The so-far unnamed victim expressed his eternal gratitude to Palaia for saving his life. Apart from a sore throat and some aching ribs, police reported that the man has since made a full recovery.
By Julie Steigerwald For Dailymail.com
Click on the link to see the video evidence of the Heimlich Manoeuvre working <Click Here>
ARAN Comment: While the rest of the world benefits from saves using abdominal thrusts, we are still waiting for one, single documented example that the ARC one-handed "chest thrusts" technique (not to be confused with the chest thrusts technique that has evidence and used in the rest of the world) has efficacy.
Children saving lives: Training towards CPR excellence levels in chest compression based on age and physical characteristics
Nicolas Mpotos, Peter Iserbyt
Resuscitation 2017 October 28, 121: 135-140
BACKGROUND: The World Health Organization's endorsement of the "Kids save lives" statement fosters the implementation of cardiopulmonary resuscitation (CPR) training for school children worldwide. However, not every child achieves and maintains the recommended chest compression depth of 5-6cm.
PURPOSE: To investigate the variability in compression depth for three age groups (grade 1: 12-14; grade 2: 14-16; grade 3: 16-18 years) as a function of physical characteristics and to define minimal compression excellence levels for training.
METHODS: Compression depth of 265 subjects (111 girls, 154 boys) aged 12-18 years from one secondary school was individually assessed and reported in percentiles per age group. Pearson correlations between physical characteristics and CPR variables were calculated. Excellence level was defined as the percentage compressions with depth 5-6cm.
RESULTS: In grade 1 (12-14 years), achieved excellence levels were 1% for girls and 23% for boys at the 75th percentile. In grade 2 (14-16 years), it increased to 24% for girls and 80% for boys. In grade 3 (16-18 years) finally, it was 59% for girls and 87% for boys. Significant positive correlations were found between CPR and physical variables (p<0.05), especially weight >50kg (p<0.01).
CONCLUSION: A minimal excellence level of 25% is achievable by boys 12-14year and girls 14-16year and can be gradually improved to 60% and 90% according to age and gender. This might necessitate more exertion and training for some younger children, especially girls, and will probably be more easily achieved for children weighing >50kg.
ARAN Comment: ARAN has long held that the ability of rescuers to perform adequate compressions in reliant on strength and mass over qualifications and experience. Other studies have shown that 46% of the Adult (>13yo) population (including health professional are able to achieve/maintain adequate chest compression depth on a typical cardiac arrest patient. ARAN is also currently conducting experiments to determine the realism on CPR manikins currently available in provided a realistic resistance to compressions. Our suspicion is that many CPR manikins (regardless of cost) give users an unrealistic sense of achievement.
Nicolas Mpotos, Peter Iserbyt
Resuscitation 2017 October 28, 121: 135-140
BACKGROUND: The World Health Organization's endorsement of the "Kids save lives" statement fosters the implementation of cardiopulmonary resuscitation (CPR) training for school children worldwide. However, not every child achieves and maintains the recommended chest compression depth of 5-6cm.
PURPOSE: To investigate the variability in compression depth for three age groups (grade 1: 12-14; grade 2: 14-16; grade 3: 16-18 years) as a function of physical characteristics and to define minimal compression excellence levels for training.
METHODS: Compression depth of 265 subjects (111 girls, 154 boys) aged 12-18 years from one secondary school was individually assessed and reported in percentiles per age group. Pearson correlations between physical characteristics and CPR variables were calculated. Excellence level was defined as the percentage compressions with depth 5-6cm.
RESULTS: In grade 1 (12-14 years), achieved excellence levels were 1% for girls and 23% for boys at the 75th percentile. In grade 2 (14-16 years), it increased to 24% for girls and 80% for boys. In grade 3 (16-18 years) finally, it was 59% for girls and 87% for boys. Significant positive correlations were found between CPR and physical variables (p<0.05), especially weight >50kg (p<0.01).
CONCLUSION: A minimal excellence level of 25% is achievable by boys 12-14year and girls 14-16year and can be gradually improved to 60% and 90% according to age and gender. This might necessitate more exertion and training for some younger children, especially girls, and will probably be more easily achieved for children weighing >50kg.
ARAN Comment: ARAN has long held that the ability of rescuers to perform adequate compressions in reliant on strength and mass over qualifications and experience. Other studies have shown that 46% of the Adult (>13yo) population (including health professional are able to achieve/maintain adequate chest compression depth on a typical cardiac arrest patient. ARAN is also currently conducting experiments to determine the realism on CPR manikins currently available in provided a realistic resistance to compressions. Our suspicion is that many CPR manikins (regardless of cost) give users an unrealistic sense of achievement.
Use of automated external defibrillators for in-hospital cardiac arrest : Any time, any place?A Wutzler, C Kloppe, A K Bilgard, A Mügge, C Hanefeld
Medizinische Klinik, Intensivmedizin und Notfallmedizin 2017 November 7
BACKGROUND: Acute treatment of in-hospital cardiac arrest (IHCA) is challenging and overall survival rates are low. However, data on the use of public-access automated external defibrillators (AEDs) for IHCA remain controversial. The aim of our study was to evaluate characteristics of patients experiencing IHCA and feasibility of public-access AED use for resuscitation in a university hospital.
METHODS: IHCA events outside the intensive care unit were analysed over a period of 21 months. Patients' characteristics, AED performance, return of spontaneous circulation (ROSC) and 24 h survival were evaluated. Outcomes following adequate and inadequate AED use were compared.
RESULTS: During the study period, 59 IHCAs occurred. AED was used in 28 (47.5%) of the cases. However, AED was adequately used in only 42.8% of total AED cases. AED use was not associated with an increased survival rate (12.9 vs. 10.7%, p = 0.8) compared to non-AED use. However, adequate AED use was associated with a higher survival rate (25 vs. 0%, p = 0.034) compared to inadequate AED use. Time from emergency call to application of AED >3 min was the most important factor of inadequate AED use. Adequate AED use was more often observed between 7:30 and 13:30 and in the internal medicine department.
CONCLUSION: AEDs were applied in less than 50% of the IHCA events. Furthermore, AED use was inadequate in the majority of the cases. Since adequate AED use is associated with improved survival, AEDs should be available in hospital areas with patients at high risk of shockable rhythm.
ARAN Comment: This study re-affirms that just having a MET team that will respond to manage all cardiac arrests is not sufficient to meet target times to first shock. AED's are once again advantageous for cardiac arrest without the need for rhythm diagnosis by clinical staff.
Medizinische Klinik, Intensivmedizin und Notfallmedizin 2017 November 7
BACKGROUND: Acute treatment of in-hospital cardiac arrest (IHCA) is challenging and overall survival rates are low. However, data on the use of public-access automated external defibrillators (AEDs) for IHCA remain controversial. The aim of our study was to evaluate characteristics of patients experiencing IHCA and feasibility of public-access AED use for resuscitation in a university hospital.
METHODS: IHCA events outside the intensive care unit were analysed over a period of 21 months. Patients' characteristics, AED performance, return of spontaneous circulation (ROSC) and 24 h survival were evaluated. Outcomes following adequate and inadequate AED use were compared.
RESULTS: During the study period, 59 IHCAs occurred. AED was used in 28 (47.5%) of the cases. However, AED was adequately used in only 42.8% of total AED cases. AED use was not associated with an increased survival rate (12.9 vs. 10.7%, p = 0.8) compared to non-AED use. However, adequate AED use was associated with a higher survival rate (25 vs. 0%, p = 0.034) compared to inadequate AED use. Time from emergency call to application of AED >3 min was the most important factor of inadequate AED use. Adequate AED use was more often observed between 7:30 and 13:30 and in the internal medicine department.
CONCLUSION: AEDs were applied in less than 50% of the IHCA events. Furthermore, AED use was inadequate in the majority of the cases. Since adequate AED use is associated with improved survival, AEDs should be available in hospital areas with patients at high risk of shockable rhythm.
ARAN Comment: This study re-affirms that just having a MET team that will respond to manage all cardiac arrests is not sufficient to meet target times to first shock. AED's are once again advantageous for cardiac arrest without the need for rhythm diagnosis by clinical staff.
Are two or four hands needed for elderly female bystanders to achieve the required chest compression depth during dispatcher-assisted CPR: a randomized controlled trial
Asta Krikscionaitiene, Zilvinas Dambrauskas, Tracey Barron, Egle Vaitkaitiene, Dinas Vaitkaitis
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2016 April 11, 24: 47
0
BACKGROUND: Rescuers are often unable to achieve the recommended 5-6 cm CC depth. The physical limitations of elderly bystanders may affect the quality of CC; thus, we investigated new strategies to improve CC performance.
METHODS: We performed a randomized controlled trial in December 2013. Sixty-eight lay rescuers aged 50-75 were randomized to intervention or control pairs (males and females separately). Each pair performed 8 min of DA-CPR on a manikin connected to a PC. Each participant in every pair took turns performing CCs in cycles of 2 min and switched as advised by the dispatcher. In the middle of every 2-min cycle, the dispatcher asked the participants of the intervention group to perform the Andrew's manoeuvre (to push on the shoulders of the person while he/she performed CCs to achieve deeper CC). Data on the quality of the CCs were analysed for each participant and pair.
RESULTS: The CC depth in the intervention group increased by 6.4 mm (p = 0.002) compared to the control group (54.2 vs. 47.8 mm) due to a significant difference in the female group. The CC depth in the female intervention and control groups was 51.5 and 44.9 mm.
DISCUSSION: The largest group of out-of-hospital cardiac arrest occurred in males over the age of 60 at home, and accordingly, the most likely witness, if any, is the spouse or family member, most frequently an older woman. There is a growing body of evidence that female rescuers are frequently unable to achieve sufficient CC depth compared to male rescuers. In some instances, the adequate depth of the CCs could only be reached using four hands, with the second pair of hands placed on the shoulders of the rescuer performing CPR.
CONCLUSION: Andrew's manoeuvre (four-hands CC) during the simulated DA-CPR significantly improved the performance of elderly female rescuers and helped them to achieve the recommended CC depth.
Asta Krikscionaitiene, Zilvinas Dambrauskas, Tracey Barron, Egle Vaitkaitiene, Dinas Vaitkaitis
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2016 April 11, 24: 47
0
BACKGROUND: Rescuers are often unable to achieve the recommended 5-6 cm CC depth. The physical limitations of elderly bystanders may affect the quality of CC; thus, we investigated new strategies to improve CC performance.
METHODS: We performed a randomized controlled trial in December 2013. Sixty-eight lay rescuers aged 50-75 were randomized to intervention or control pairs (males and females separately). Each pair performed 8 min of DA-CPR on a manikin connected to a PC. Each participant in every pair took turns performing CCs in cycles of 2 min and switched as advised by the dispatcher. In the middle of every 2-min cycle, the dispatcher asked the participants of the intervention group to perform the Andrew's manoeuvre (to push on the shoulders of the person while he/she performed CCs to achieve deeper CC). Data on the quality of the CCs were analysed for each participant and pair.
RESULTS: The CC depth in the intervention group increased by 6.4 mm (p = 0.002) compared to the control group (54.2 vs. 47.8 mm) due to a significant difference in the female group. The CC depth in the female intervention and control groups was 51.5 and 44.9 mm.
DISCUSSION: The largest group of out-of-hospital cardiac arrest occurred in males over the age of 60 at home, and accordingly, the most likely witness, if any, is the spouse or family member, most frequently an older woman. There is a growing body of evidence that female rescuers are frequently unable to achieve sufficient CC depth compared to male rescuers. In some instances, the adequate depth of the CCs could only be reached using four hands, with the second pair of hands placed on the shoulders of the rescuer performing CPR.
CONCLUSION: Andrew's manoeuvre (four-hands CC) during the simulated DA-CPR significantly improved the performance of elderly female rescuers and helped them to achieve the recommended CC depth.
ARAN Comment: Alternative techniques like the Andrew Manoeuvre and Pedal Compressions are effective alternatives for those who lack the body mass/strength or have disabilities/injuries restricted then from using the traditional kneeling technique. The insistence by the ARC on only using the kneeling technique for resuscitation does not reflect the reality of those who may be called upon to provide OHCA compressions. This dogmatic position has likely cost many lives.
Scand J Trauma Resusc Emerg Med. 2016 Apr 11;24:47. doi: 10.1186/s13049-016-0238-z.
Are two or four hands needed for elderly female bystanders to achieve the required chest compression depth during dispatcher-assisted CPR: a randomized controlled trial.
Krikscionaitiene A1, Dambrauskas Z2, Barron T3, Vaitkaitiene E4, Vaitkaitis D4
Four hands are needed for female bystanders to achieve the required chest compression depth during dispatcher assisted CPR: A randomized controlled trial
Asta Krikscionaitiene, Dinas Vaitkaitis, Zilvinas Dambrauskas, Tracey Barron, BS and Egle Vaitkaitiene
Aug 1, 2015 | 2015, AEDR 2015 Vol. 3 Issue 2, Research Posters
Scand J Trauma Resusc Emerg Med. 2016 Apr 11;24:47. doi: 10.1186/s13049-016-0238-z.
Are two or four hands needed for elderly female bystanders to achieve the required chest compression depth during dispatcher-assisted CPR: a randomized controlled trial.
Krikscionaitiene A1, Dambrauskas Z2, Barron T3, Vaitkaitiene E4, Vaitkaitis D4
Four hands are needed for female bystanders to achieve the required chest compression depth during dispatcher assisted CPR: A randomized controlled trial
Asta Krikscionaitiene, Dinas Vaitkaitis, Zilvinas Dambrauskas, Tracey Barron, BS and Egle Vaitkaitiene
Aug 1, 2015 | 2015, AEDR 2015 Vol. 3 Issue 2, Research Posters
Easy-to-learn cardiopulmonary resuscitation training programme: a randomised controlled trial on laypeople's resuscitation performance
Rachel Jia Min Ko, Swee Han Lim, Vivien Xi Wu, Tak Yam Leong, Sok Ying Liaw
Singapore Medical Journal 2017 November 13
INTRODUCTION: Simplifying the learning of cardiopulmonary resuscitation (CPR) is advocated to improve skill acquisition and retention. A simplified CPR training programme focusing on continuous chest compression, with a simple landmark tracing technique, was introduced to laypeople. The study aimed to examine the effectiveness of the simplified CPR training in improving lay rescuers' CPR performance as compared to standard CPR.
METHODS: 85 laypeople (aged 21-60 years) were recruited and randomly assigned to undertake either a two-hour simplified CPR training or standard CPR training. They were tested two months after the training on a simulated cardiac arrest scenario. The participant's performance on the sequence of CPR steps was observed and evaluated using a validated CPR algorithm checklist. The quality of chest compression and ventilation were assessed from the recording manikins.
RESULTS: The simplified CPR group performed significantly better on the CPR algorithm when compared to the standard CPR group (p < 0.01). No significant difference was found between the groups on the time to initiate CPR. However, a significantly higher number of compressions and proportion of adequate compressions was demonstrated by the simplified group than the standard group (p < 0.01). Hands-off time was significantly shorter in the simplified CPR group than in the standard CPR group (p < 0.001).
CONCLUSION: Simplifying the learning of CPR by focusing on continuous chest compressions, with simple hand placement for chest compression, could lead to better acquisition and retention of the CPR algorithms, and better quality of chest compressions than standard CPR.
ARAN Comment: Yet another study indicating the superiority of compression-only CPR for bystander CPR (using BLS). Supports the obvious truth i.e. that in the pre-ambulance period in SCA, compression-only CPR (for BLS providers) is better in both willingness of the public and outcome for casualties. Let's just stop treating all cardiac arrests as hypoxic arrests! To do so is not supported by science. Unfortunately recalcitrance in Australia is leading to poorer outcomes.
Rachel Jia Min Ko, Swee Han Lim, Vivien Xi Wu, Tak Yam Leong, Sok Ying Liaw
Singapore Medical Journal 2017 November 13
INTRODUCTION: Simplifying the learning of cardiopulmonary resuscitation (CPR) is advocated to improve skill acquisition and retention. A simplified CPR training programme focusing on continuous chest compression, with a simple landmark tracing technique, was introduced to laypeople. The study aimed to examine the effectiveness of the simplified CPR training in improving lay rescuers' CPR performance as compared to standard CPR.
METHODS: 85 laypeople (aged 21-60 years) were recruited and randomly assigned to undertake either a two-hour simplified CPR training or standard CPR training. They were tested two months after the training on a simulated cardiac arrest scenario. The participant's performance on the sequence of CPR steps was observed and evaluated using a validated CPR algorithm checklist. The quality of chest compression and ventilation were assessed from the recording manikins.
RESULTS: The simplified CPR group performed significantly better on the CPR algorithm when compared to the standard CPR group (p < 0.01). No significant difference was found between the groups on the time to initiate CPR. However, a significantly higher number of compressions and proportion of adequate compressions was demonstrated by the simplified group than the standard group (p < 0.01). Hands-off time was significantly shorter in the simplified CPR group than in the standard CPR group (p < 0.001).
CONCLUSION: Simplifying the learning of CPR by focusing on continuous chest compressions, with simple hand placement for chest compression, could lead to better acquisition and retention of the CPR algorithms, and better quality of chest compressions than standard CPR.
ARAN Comment: Yet another study indicating the superiority of compression-only CPR for bystander CPR (using BLS). Supports the obvious truth i.e. that in the pre-ambulance period in SCA, compression-only CPR (for BLS providers) is better in both willingness of the public and outcome for casualties. Let's just stop treating all cardiac arrests as hypoxic arrests! To do so is not supported by science. Unfortunately recalcitrance in Australia is leading to poorer outcomes.
The IOs have it: a prospective observational study of vascular access success rates in patients in extremis using video review Kristen M Chreiman, Ryan P Dumas, Mark J Seamon, Patrick K Kim, Patrick M Reilly, Lewis J Kaplan, Jason D Christie, Daniel N Holena
Journal of Trauma and Acute Care Surgery 2018 January 4
BACKGROUND: Quick and successful vascular access in injured patients arriving in extremis is crucial to enable early resuscitation and rapid OR transport for definitive repair. We hypothesized that intraosseous (IO) access would be faster and have higher success rates than peripheral IVs (PIVs) or central venous catheters (CVCs).
METHODS: High-definition video recordings of resuscitations for all patients undergoing Emergency Department Thoracotomy (EDT) from 4/2016-7/2017 were reviewed as part of a quality improvement initiative. Demographics, mechanism of injury, access type, access location, start and stop time, and success of each vascular access attempt were recorded. Times to completion for access types (PIV, IO, CVC) were compared using Kruskal-Wallis test adjusted for multiple comparisons while categorical outcomes such as success rates by access type were compared using chi-squared test or Fisher's exact test.
RESULTS: Study patients had a median age of 30 (IQR 25-38), were 92% male, 92% African American, and 93% sustained penetrating trauma. A total of 145 access attempts in 38 patients occurred (median 3.8 (SD 1.4) attempts per patient). There was no difference between duration of PIV and IO attempts (0.63 IQR 0.35-0.96 vs. 0.39 IQR 0.13-0.65 minutes, adjusted p = 0.03), but both PIV and IO were faster than CVC attempts (3.2 IQR 1.72 - 5.23 minutes, adjusted p<0.001 for both comparisons). Intraosseous lines had higher success rates than PIVs or CVCs (95% vs. 42% vs. 46%, p<0.001).
CONCLUSIONS: Access attempts using IO are as fast as PIV attempts but are more than twice as likely to be successful. Attempts at CVC access in patients in extremis have high rates of failure and take a median of over 3 minutes. While IO access may not completely supplant PIVs and CVCs, IO access should be considered as a first line therapy for trauma patients in extremis.
Journal of Trauma and Acute Care Surgery 2018 January 4
BACKGROUND: Quick and successful vascular access in injured patients arriving in extremis is crucial to enable early resuscitation and rapid OR transport for definitive repair. We hypothesized that intraosseous (IO) access would be faster and have higher success rates than peripheral IVs (PIVs) or central venous catheters (CVCs).
METHODS: High-definition video recordings of resuscitations for all patients undergoing Emergency Department Thoracotomy (EDT) from 4/2016-7/2017 were reviewed as part of a quality improvement initiative. Demographics, mechanism of injury, access type, access location, start and stop time, and success of each vascular access attempt were recorded. Times to completion for access types (PIV, IO, CVC) were compared using Kruskal-Wallis test adjusted for multiple comparisons while categorical outcomes such as success rates by access type were compared using chi-squared test or Fisher's exact test.
RESULTS: Study patients had a median age of 30 (IQR 25-38), were 92% male, 92% African American, and 93% sustained penetrating trauma. A total of 145 access attempts in 38 patients occurred (median 3.8 (SD 1.4) attempts per patient). There was no difference between duration of PIV and IO attempts (0.63 IQR 0.35-0.96 vs. 0.39 IQR 0.13-0.65 minutes, adjusted p = 0.03), but both PIV and IO were faster than CVC attempts (3.2 IQR 1.72 - 5.23 minutes, adjusted p<0.001 for both comparisons). Intraosseous lines had higher success rates than PIVs or CVCs (95% vs. 42% vs. 46%, p<0.001).
CONCLUSIONS: Access attempts using IO are as fast as PIV attempts but are more than twice as likely to be successful. Attempts at CVC access in patients in extremis have high rates of failure and take a median of over 3 minutes. While IO access may not completely supplant PIVs and CVCs, IO access should be considered as a first line therapy for trauma patients in extremis.
Great to see the first public education campaign about CPR in Australia. (click here)
The ABC has produced Australia's first public education television advertisement about the importance of bystander steps in the event of a cardiac arrest. ARAN has been advocating for this for some time at state and federal level to focus the public on the truth of SCA. It is also great to see that at last our message has got through about Sudden Cardiac Arrest i.e. the only actions that make a difference are calling for help, starting fast and deep compressions and using a defibrillator. Finally the dogma of ventilations in SCA has been dropped from the message. Kudos to the Tasmanian Branch of the ARC who have shown innovation and common sense in presenting the public with the right message, I am sure they have had to overcome resistance from the ARC National Council.
Sad and angry!
When 3 yo Tasmanian boy choked to death recently in his mother's arms, we were all deeply saddened for this tragic loss of life. His mother (who was trained in all the current Australian first aid measures) tried in vain to remove the ball from his airway and commenced CPR waiting for Paramedics. She did everything she was told to but was tragically unable to save her son.
This situation is not only tragic but frustrating and makes us here at ARAN very angry. ARAN has been warning the ARC for many years about what will happen if people use their choking guidelines, guidelines that differ from the rest of the world. Not because they are better and more effective but because the ARC says so! from our own experience, anyone who challenges their choking guidelines and the evidence and science behind them is ostracised, belittled, white-anted and has court action threatened against them. We have consistently asked the ARC to prove what they say, including:
This situation is not only tragic but frustrating and makes us here at ARAN very angry. ARAN has been warning the ARC for many years about what will happen if people use their choking guidelines, guidelines that differ from the rest of the world. Not because they are better and more effective but because the ARC says so! from our own experience, anyone who challenges their choking guidelines and the evidence and science behind them is ostracised, belittled, white-anted and has court action threatened against them. We have consistently asked the ARC to prove what they say, including:
- Where is the evidence for their "one-handed chest thrusts" technique that they recommend instead of abdominal thrusts that are use in every other country in the world?
- Where are the studies and clinical trials that prove their recommendations are better and more effective than every country in the world and backed by their experts?
- Why has there been no reported saves from the ARC technique in 15 years (since its inception), despite abdominal thrusts saving lives daily around the world?
- Why does the ARC perpetuate the myth that their "chest thrust" technique has the same efficacy as the American "chest thrusts" technique when they are two completely different methods (the US one having studies behind it)?
- Where is the evidence of all the injured and dead people who have been "inflicted" with abdominal thrusts over the years?
- Why does the ARC act with apparent impunity when their guidelines fail to provide the outcomes that are realised in the rest of world?
Impact of Bystander Automated External Defibrillator Use on Survival and Functional Outcomes in Shockable Observed Public Cardiac Arrests
Ross A Pollack, Siobhan P Brown, Thomas Rea, Tom Aufderheide, David Barbic, Jason E Buick, James Christenson, Ahamed H Idris, Jamie Jasti, Michael Kampp, Peter Kudenchuk, Susanne May, Marc Muhr, Graham Nichol, Joseph P Ornato, George Sopko, Christian Vaillancourt, Laurie Morrison, Myron Weisfeldt
Circulation 2018 February 26
"Patients shocked by a bystander were significantly more likely to survive to discharge (66.5% versus 43.0%) and be discharged with favourable functional outcome (57.1% versus 32.7%) than patients initially shocked by emergency medical services."
The use of BMV compared with ETI failed to demonstrate noninferiority or inferiority for survival with favorable 28-day neurological function
Effect of Bag-Mask Ventilation vs Endotracheal Intubation During Cardiopulmonary Resuscitation on Neurological Outcome After Out-of-Hospital Cardiorespiratory Arrest: A Randomized Clinical Trial
Patricia Jabre, Andrea Penaloza, David Pinero, Francois-Xavier Duchateau, Stephen W Borron, Francois Javaudin, Olivier Richard, Diane de Longueville, Guillem Bouilleau, Marie-Laure Devaud, Matthieu Heidet, Caroline Lejeune, Sophie Fauroux, Jean-Luc Greingor, Alessandro Manara, Jean-Christophe Hubert, Bertrand Guihard, Olivier Vermylen, Pascale Lievens, Yannick Auffret, Celine Maisondieu, Stephanie Huet, Benoît Claessens, Frederic Lapostolle, Nicolas Javaud, Paul-Georges Reuter, Elinor Baker, Eric Vicaut, Frédéric Adnet
JAMA: the Journal of the American Medical Association 2018 February 27, 319 (8): 779-787
Importance: Bag-mask ventilation (BMV) is a less complex technique than endotracheal intubation (ETI) for airway management during the advanced cardiac life support phase of cardiopulmonary resuscitation of patients with out-of-hospital cardiorespiratory arrest. It has been reported as superior in terms of survival.
Objectives: To assess noninferiority of BMV vs ETI for advanced airway management with regard to survival with favorable neurological function at day 28.
Design, Settings, and Participants: Multicenter randomized clinical trial comparing BMV with ETI in 2043 patients with out-of-hospital cardiorespiratory arrest in France and Belgium. Enrollment occurred from March 9, 2015, to January 2, 2017, and follow-up ended January 26, 2017.
Intervention: Participants were randomized to initial airway management with BMV (n = 1020) or ETI (n = 1023).
Main Outcomes and Measures: The primary outcome was favorable neurological outcome at 28 days defined as cerebral performance category 1 or 2. A noninferiority margin of 1% was chosen. Secondary end points included rate of survival to hospital admission, rate of survival at day 28, rate of return of spontaneous circulation, and ETI and BMV difficulty or failure.
Results: Among 2043 patients who were randomized (mean age, 64.7 years; 665 women [32%]), 2040 (99.8%) completed the trial. In the intention-to-treat population, favorable functional survival at day 28 was 44 of 1018 patients (4.3%) in the BMV group and 43 of 1022 patients (4.2%) in the ETI group (difference, 0.11% [1-sided 97.5% CI, -1.64% to infinity]; P for noninferiority = .11). Survival to hospital admission (294/1018 [28.9%] in the BMV group vs 333/1022 [32.6%] in the ETI group; difference, -3.7% [95% CI, -7.7% to 0.3%]) and global survival at day 28 (55/1018 [5.4%] in the BMV group vs 54/1022 [5.3%] in the ETI group; difference, 0.1% [95% CI, -1.8% to 2.1%]) were not significantly different. Complications included difficult airway management (186/1027 [18.1%] in the BMV group vs 134/996 [13.4%] in the ETI group; difference, 4.7% [95% CI, 1.5% to 7.9%]; P = .004), failure (69/1028 [6.7%] in the BMV group vs 21/996 [2.1%] in the ETI group; difference, 4.6% [95% CI, 2.8% to 6.4%]; P < .001), and regurgitation of gastric content (156/1027 [15.2%] in the BMV group vs 75/999 [7.5%] in the ETI group; difference, 7.7% [95% CI, 4.9% to 10.4%]; P < .001).
Conclusions and Relevance: Among patients with out-of-hospital cardiorespiratory arrest, the use of BMV compared with ETI failed to demonstrate noninferiority or inferiority for survival with favorable 28-day neurological function, an inconclusive result. A determination of equivalence or superiority between these techniques requires further research.
Patricia Jabre, Andrea Penaloza, David Pinero, Francois-Xavier Duchateau, Stephen W Borron, Francois Javaudin, Olivier Richard, Diane de Longueville, Guillem Bouilleau, Marie-Laure Devaud, Matthieu Heidet, Caroline Lejeune, Sophie Fauroux, Jean-Luc Greingor, Alessandro Manara, Jean-Christophe Hubert, Bertrand Guihard, Olivier Vermylen, Pascale Lievens, Yannick Auffret, Celine Maisondieu, Stephanie Huet, Benoît Claessens, Frederic Lapostolle, Nicolas Javaud, Paul-Georges Reuter, Elinor Baker, Eric Vicaut, Frédéric Adnet
JAMA: the Journal of the American Medical Association 2018 February 27, 319 (8): 779-787
Importance: Bag-mask ventilation (BMV) is a less complex technique than endotracheal intubation (ETI) for airway management during the advanced cardiac life support phase of cardiopulmonary resuscitation of patients with out-of-hospital cardiorespiratory arrest. It has been reported as superior in terms of survival.
Objectives: To assess noninferiority of BMV vs ETI for advanced airway management with regard to survival with favorable neurological function at day 28.
Design, Settings, and Participants: Multicenter randomized clinical trial comparing BMV with ETI in 2043 patients with out-of-hospital cardiorespiratory arrest in France and Belgium. Enrollment occurred from March 9, 2015, to January 2, 2017, and follow-up ended January 26, 2017.
Intervention: Participants were randomized to initial airway management with BMV (n = 1020) or ETI (n = 1023).
Main Outcomes and Measures: The primary outcome was favorable neurological outcome at 28 days defined as cerebral performance category 1 or 2. A noninferiority margin of 1% was chosen. Secondary end points included rate of survival to hospital admission, rate of survival at day 28, rate of return of spontaneous circulation, and ETI and BMV difficulty or failure.
Results: Among 2043 patients who were randomized (mean age, 64.7 years; 665 women [32%]), 2040 (99.8%) completed the trial. In the intention-to-treat population, favorable functional survival at day 28 was 44 of 1018 patients (4.3%) in the BMV group and 43 of 1022 patients (4.2%) in the ETI group (difference, 0.11% [1-sided 97.5% CI, -1.64% to infinity]; P for noninferiority = .11). Survival to hospital admission (294/1018 [28.9%] in the BMV group vs 333/1022 [32.6%] in the ETI group; difference, -3.7% [95% CI, -7.7% to 0.3%]) and global survival at day 28 (55/1018 [5.4%] in the BMV group vs 54/1022 [5.3%] in the ETI group; difference, 0.1% [95% CI, -1.8% to 2.1%]) were not significantly different. Complications included difficult airway management (186/1027 [18.1%] in the BMV group vs 134/996 [13.4%] in the ETI group; difference, 4.7% [95% CI, 1.5% to 7.9%]; P = .004), failure (69/1028 [6.7%] in the BMV group vs 21/996 [2.1%] in the ETI group; difference, 4.6% [95% CI, 2.8% to 6.4%]; P < .001), and regurgitation of gastric content (156/1027 [15.2%] in the BMV group vs 75/999 [7.5%] in the ETI group; difference, 7.7% [95% CI, 4.9% to 10.4%]; P < .001).
Conclusions and Relevance: Among patients with out-of-hospital cardiorespiratory arrest, the use of BMV compared with ETI failed to demonstrate noninferiority or inferiority for survival with favorable 28-day neurological function, an inconclusive result. A determination of equivalence or superiority between these techniques requires further research.
Study shows abdominal thrusts are safe and effective and singles out Australia as being out of touch with latest research.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5520267/www.ncbi.nlm.nih.gov/pmc/articles/PMC5520267/
Modern Approach to Basic Airway Management
Sun, Apr 1, 2018 JEMS
By Andrew Merelman, BS, NRP, FP-C , Richard Levitan, MD, FACEP
Excerpts from a recent JEMS article describing a modern approach to the essentials of ventilation & oxygenation.
Sun, Apr 1, 2018 JEMS
By Andrew Merelman, BS, NRP, FP-C , Richard Levitan, MD, FACEP
Excerpts from a recent JEMS article describing a modern approach to the essentials of ventilation & oxygenation.
VENTILATION
Ventilation is often the most important intervention being performed, & doing it correctly should be a priority.
The reality is that ventilation is often the most important intervention being performed, and doing it correctly should be a priority. Without conscious awareness, the tendency is for providers to ventilate too fast and with excessive volume.
Proper BVM technique is composed of three main principles: 1) consistent mask seal; 2) proper tidal volume; and, 3) controlled rate. Mask seal is best optimized by using a two-person technique.
Ventilation is often the most important intervention being performed, & doing it correctly should be a priority.
The reality is that ventilation is often the most important intervention being performed, and doing it correctly should be a priority. Without conscious awareness, the tendency is for providers to ventilate too fast and with excessive volume.
Proper BVM technique is composed of three main principles: 1) consistent mask seal; 2) proper tidal volume; and, 3) controlled rate. Mask seal is best optimized by using a two-person technique.
Two person technique for ventilation showing jaw thrust
When a one-person technique is necessary, “C-E” is the best option for mask seal. The biggest detriment to the “C-E” technique is that the provider only has their pinky and ring fingers available to perform a jaw thrust. These fingers are weaker and can’t easily displace the jaw to open the airway.
After the mask seal, squeezing the bag properly is the other critical component of BVM use. A standard adult BVM has a volume of about 1,000–1,200 mL. Most adult patients only need around 400-500 mL of volume delivered in each breath. This means that providers should use one hand and attempt to only squeeze about half or less of the volume of the bag in each breath.Using lower volumes and squeezing slowly also reduces the chance of filling the stomach with air and causing vomiting. One way to ensure more appropriate tidal volumes is to use a pediatric BVM for adult patients. They generally provide a volume of 400–600 mL, which is perfect for adults.
Additionally, the person squeezing the bag must consciously limit the ventilatory rate to avoid over-ventilation. It’s common to see providers over-ventilating as they aren’t focused on the task and are under an adrenaline surge.
SUPRAGLOTTIC DEVICES
One of the most important recent developments in airway management is modern supraglottic devices. They’ve evolved quickly, and today, they are more effective and easier to insert than ever before—so much so that many surgical procedures under general anesthesia are being performed with laryngeal mask devices in lieu of endotracheal intubation.
The most revolutionary of these devices is the laryngeal mask style airways. The third and fourth generation devices of this type have improved mask design, and are made to function under patient movement and with secretions in the airway. Additionally, they’re easier to insert than older laryngeal mask devices or other supraglottic airways.
These modern airway adjuncts have changed the way we approach BVM ventilation. We know that ventilating with a mask is often difficult and can cause gastric distention. In patients who can tolerate it and don’t have an intact gag reflex, a laryngeal mask airway should be utilized when BVM ventilation is necessary. Inserting the device is quick and easy, and it allows more definitive and effective ventilation and airway control. It eliminates the need for a handheld mask seal while significantly lowering the risk of gastric insufflation and vomiting. In fact, upper airway collapse actually improves laryngeal mask functionality as the airway tissues collapse into the bowl and improve the mask seal. These principles are also true in cardiac arrest. If a BVM is going to be used, placing a laryngeal mask is beneficial.
REFERENCES
1. Fouke JM, Strohl KP. Effect of position and lung volume on upper airway geometry. J Appl Physiol. 1987;63(1):375–380.
2. Levitan R. (Jan 11, 2017.) Should emergency physicians abandon face-mask ventilation? ACEP Now. Retrieved Feb. 17, 2018, from www.acepnow.com/article/ emergency-physicians-abandon-face-mask-ventilation.
3. Levitan R. (2013). The neglected orifice. Emergency Physicians Monthly. Retrieved Feb. 17, 2018 from www.epmonthly.com/article/the-neglected-orifice/.
4. Weingart S, Levitan, R. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165–175
5. Brindley PG, Beed M, Law JA, et al. Airway management outside the operating room: How to better prepare. Can J Anaesth. 2017;64(5):530–539
6. Brown DJ, Carroll SM, April MD. Face mask leak with nasal cannula during noninvasive positive pressure ventilation: A randomized crossover trial. Am J Emerg Med. Dec. 2, 2017. [Epub ahead of print.]
7. Siegler J, Kroll M, Wojcik S, et al. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp Emerg Care. 2017;21(1):74–78.
8. Khoury A, Sall FS, De Luca A, et al. Evaluation of bag-valve-mask ventilation in manikin studies: What are the current limitations? Biomed Res Int. 2016;2016:4521767.
After the mask seal, squeezing the bag properly is the other critical component of BVM use. A standard adult BVM has a volume of about 1,000–1,200 mL. Most adult patients only need around 400-500 mL of volume delivered in each breath. This means that providers should use one hand and attempt to only squeeze about half or less of the volume of the bag in each breath.Using lower volumes and squeezing slowly also reduces the chance of filling the stomach with air and causing vomiting. One way to ensure more appropriate tidal volumes is to use a pediatric BVM for adult patients. They generally provide a volume of 400–600 mL, which is perfect for adults.
Additionally, the person squeezing the bag must consciously limit the ventilatory rate to avoid over-ventilation. It’s common to see providers over-ventilating as they aren’t focused on the task and are under an adrenaline surge.
SUPRAGLOTTIC DEVICES
One of the most important recent developments in airway management is modern supraglottic devices. They’ve evolved quickly, and today, they are more effective and easier to insert than ever before—so much so that many surgical procedures under general anesthesia are being performed with laryngeal mask devices in lieu of endotracheal intubation.
The most revolutionary of these devices is the laryngeal mask style airways. The third and fourth generation devices of this type have improved mask design, and are made to function under patient movement and with secretions in the airway. Additionally, they’re easier to insert than older laryngeal mask devices or other supraglottic airways.
These modern airway adjuncts have changed the way we approach BVM ventilation. We know that ventilating with a mask is often difficult and can cause gastric distention. In patients who can tolerate it and don’t have an intact gag reflex, a laryngeal mask airway should be utilized when BVM ventilation is necessary. Inserting the device is quick and easy, and it allows more definitive and effective ventilation and airway control. It eliminates the need for a handheld mask seal while significantly lowering the risk of gastric insufflation and vomiting. In fact, upper airway collapse actually improves laryngeal mask functionality as the airway tissues collapse into the bowl and improve the mask seal. These principles are also true in cardiac arrest. If a BVM is going to be used, placing a laryngeal mask is beneficial.
REFERENCES
1. Fouke JM, Strohl KP. Effect of position and lung volume on upper airway geometry. J Appl Physiol. 1987;63(1):375–380.
2. Levitan R. (Jan 11, 2017.) Should emergency physicians abandon face-mask ventilation? ACEP Now. Retrieved Feb. 17, 2018, from www.acepnow.com/article/ emergency-physicians-abandon-face-mask-ventilation.
3. Levitan R. (2013). The neglected orifice. Emergency Physicians Monthly. Retrieved Feb. 17, 2018 from www.epmonthly.com/article/the-neglected-orifice/.
4. Weingart S, Levitan, R. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59(3):165–175
5. Brindley PG, Beed M, Law JA, et al. Airway management outside the operating room: How to better prepare. Can J Anaesth. 2017;64(5):530–539
6. Brown DJ, Carroll SM, April MD. Face mask leak with nasal cannula during noninvasive positive pressure ventilation: A randomized crossover trial. Am J Emerg Med. Dec. 2, 2017. [Epub ahead of print.]
7. Siegler J, Kroll M, Wojcik S, et al. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp Emerg Care. 2017;21(1):74–78.
8. Khoury A, Sall FS, De Luca A, et al. Evaluation of bag-valve-mask ventilation in manikin studies: What are the current limitations? Biomed Res Int. 2016;2016:4521767.
Acting on the Call
New Global initiative to improve Out of Hospital Cardiac Arrests rates by focusing on the key elements, especially in the community.
New Global initiative to improve Out of Hospital Cardiac Arrests rates by focusing on the key elements, especially in the community.
Advanced vs. Basic Life Support in the Treatment of Out-of-Hospital Cardiopulmonary Arrest in the Resuscitation Outcomes Consortium
Michael Christopher Kurz, Robert H Schmicker, Brian Leroux, Graham Nichol, Tom P Aufderheide, Sheldon Cheskes, Brian Grunau, Jamie Jasti, Peter Kudenchuk, Gary M Vilke, Jason Buick, Lynn Wittwer, Ritu Sahni, Ronald Straight, Henry E Wang
Resuscitation 2018 April 30
BACKGROUND: Prior observational studies suggest no additional benefit from advanced life support (ALS) when compared with providing basic life support (BLS) for patients with out-of-hospital cardiac arrest (OHCA). We compared the association of ALS care with OHCA outcomes using prospective clinical data from the Resuscitation Outcomes Consortium (ROC).
METHODS: Included were consecutive adults OHCA treated by participating emergency medical services (EMS) agencies between June 1, 2011, and June 30, 2015. We defined BLS as receipt of cardiopulmonary resuscitation (CPR) and/or automated defibrillation and ALS as receipt of an advanced airway, manual defibrillation, or intravenous drug therapy. We compared outcomes among patients receiving: 1) BLS-only; 2) BLS + late ALS; 3) BLS + early ALS; and 4) ALS-first care. Using multivariable logistic regression, we evaluated the associations between level of care and return of spontaneous circulation (ROSC), survival to hospital discharge, and survival with good functional status, adjusting for age, sex, witnessed arrest, bystander CPR, shockable initial rhythm, public location, EMS response time, CPR quality, and ROC site.
RESULTS: Among 35,065 patients with OHCA, characteristics were median age 68 years (IQR 56-80), male 63.9%, witnessed arrest 43.8%, bystander CPR 50.6%, and shockable initial rhythm 24.2%. Care delivered was: 4.0% BLS-only, 31.5% BLS + late ALS, 17.2% BLS + early ALS, and 47.3% ALS-first. ALS care with or without initial BLS care was independently associated with increased adjusted ROSC and survival to hospital discharge unless delivered greater than 6 minutes after BLS arrival (BLS + late ALS). Regardless of when it was delivered, ALS care was not associated with significantly greater functional outcome.
CONCLUSION: ALS care was associated with survival to hospital discharge when provided initially or within six minutes of BLS arrival. ALS care, with or without initial BLS care, was associated with increased ROSC, however it was not associated with functional outcome.
Michael Christopher Kurz, Robert H Schmicker, Brian Leroux, Graham Nichol, Tom P Aufderheide, Sheldon Cheskes, Brian Grunau, Jamie Jasti, Peter Kudenchuk, Gary M Vilke, Jason Buick, Lynn Wittwer, Ritu Sahni, Ronald Straight, Henry E Wang
Resuscitation 2018 April 30
BACKGROUND: Prior observational studies suggest no additional benefit from advanced life support (ALS) when compared with providing basic life support (BLS) for patients with out-of-hospital cardiac arrest (OHCA). We compared the association of ALS care with OHCA outcomes using prospective clinical data from the Resuscitation Outcomes Consortium (ROC).
METHODS: Included were consecutive adults OHCA treated by participating emergency medical services (EMS) agencies between June 1, 2011, and June 30, 2015. We defined BLS as receipt of cardiopulmonary resuscitation (CPR) and/or automated defibrillation and ALS as receipt of an advanced airway, manual defibrillation, or intravenous drug therapy. We compared outcomes among patients receiving: 1) BLS-only; 2) BLS + late ALS; 3) BLS + early ALS; and 4) ALS-first care. Using multivariable logistic regression, we evaluated the associations between level of care and return of spontaneous circulation (ROSC), survival to hospital discharge, and survival with good functional status, adjusting for age, sex, witnessed arrest, bystander CPR, shockable initial rhythm, public location, EMS response time, CPR quality, and ROC site.
RESULTS: Among 35,065 patients with OHCA, characteristics were median age 68 years (IQR 56-80), male 63.9%, witnessed arrest 43.8%, bystander CPR 50.6%, and shockable initial rhythm 24.2%. Care delivered was: 4.0% BLS-only, 31.5% BLS + late ALS, 17.2% BLS + early ALS, and 47.3% ALS-first. ALS care with or without initial BLS care was independently associated with increased adjusted ROSC and survival to hospital discharge unless delivered greater than 6 minutes after BLS arrival (BLS + late ALS). Regardless of when it was delivered, ALS care was not associated with significantly greater functional outcome.
CONCLUSION: ALS care was associated with survival to hospital discharge when provided initially or within six minutes of BLS arrival. ALS care, with or without initial BLS care, was associated with increased ROSC, however it was not associated with functional outcome.
Great to see that (at last) the message about SCA from the ERC that we have been promoting since the inception of ARAN is finally gaining mainstream support in Australia i.e. CALL - PUSH - SHOCK, the only 3 proven measures in SCA in BLS.
- Call 000 – follow the instructions
- Push – link hands, push hard and fast
- Shock – use an AED
How useful is CPR during ambulance transport?
In a retrospective analysis of a registry of out-of-hospital cardiac arrest (OHCA) cases treated between 2008 and 2014, only 259 (3.6%) of OHCA in patients received cardiopulmonary resuscitation (CPR) during ambulance transport. The included patients who had not ROSC at the time it was decided to transport to a hospital and who were rejected as non-heart-beating donors. Factors as young patient age, cardiac arrest outside the home, the presence of a witness, lack of a shockable rhythm on responder arrival, lack of BLS prior to responder arrival, non-cardiac cause, and orotracheal intubation are associated with the use of ambulance CPR, a strategy that can be considered futile because nearly nobody survived.
Comments: Should we stop performing CPR during ambulance transport? Only 1 in 259 (0.38%) victims of OHCA with CPR during ambulance transport survived to discharge with good neurologic outcome. However, not doing this would not have kept that one person alive.
Rosell Ortiz F, García Del Águila J, Fernández Del Valle P, J Mellado-Vergel F, Vergara-Pérez S, R Ruiz-Montero M, Martínez-Lara M et al. Ambulance cardiopulmonary resuscitation: outcomes and associated factors in out-of-hospital cardiac arrest. Emergencias. 2018 Jun;30(3):156-162. [Article in English, Spanish; Abstract available in Spanish from the publisher]
In a retrospective analysis of a registry of out-of-hospital cardiac arrest (OHCA) cases treated between 2008 and 2014, only 259 (3.6%) of OHCA in patients received cardiopulmonary resuscitation (CPR) during ambulance transport. The included patients who had not ROSC at the time it was decided to transport to a hospital and who were rejected as non-heart-beating donors. Factors as young patient age, cardiac arrest outside the home, the presence of a witness, lack of a shockable rhythm on responder arrival, lack of BLS prior to responder arrival, non-cardiac cause, and orotracheal intubation are associated with the use of ambulance CPR, a strategy that can be considered futile because nearly nobody survived.
Comments: Should we stop performing CPR during ambulance transport? Only 1 in 259 (0.38%) victims of OHCA with CPR during ambulance transport survived to discharge with good neurologic outcome. However, not doing this would not have kept that one person alive.
Rosell Ortiz F, García Del Águila J, Fernández Del Valle P, J Mellado-Vergel F, Vergara-Pérez S, R Ruiz-Montero M, Martínez-Lara M et al. Ambulance cardiopulmonary resuscitation: outcomes and associated factors in out-of-hospital cardiac arrest. Emergencias. 2018 Jun;30(3):156-162. [Article in English, Spanish; Abstract available in Spanish from the publisher]
Please support a petition to conduct a Royal Commission into the NSW Ambulance Service
AHA: Hands-Only CPR Training Kiosks as Effective as Class Setting
While ARAN has been advocating for Hands-Only CPR kiosks at airports in Australia but has faced road blocks and resistance from multiple quarters, the AHA has a released its findings that these kiosks (that have trained 100,00 travellers in the US) are as effective as a 30 minute face-to-face CPR session.
The US has figured out that the most common cardiac arrest is an SCA and compressions-only are the appropriate intervention. Hypoxic arrests are the exception. In Australia all arrests are presumed to be drownings in young people, but this is very rare.
Minimum depth and rates of compressions are just not good enough...
Association between Pre-hospital CPR Quality and End-Tidal Carbon Dioxide Levels in Out-of-Hospital Cardiac Arrest
Ryan A. Murphy , MD,Bentley J. Bobrow , MD,Daniel W. Spaite , MD,Chengcheng Hu , PhD,Robyn McDannold , MS &Tyler F. Vadeboncoeur , MD, Pages 369-377 | Published online: 01 Feb 2016
Introduction: International Guidelines recommend measurement of end-tidal carbon dioxide (EtCO2) to enhance cardiopulmonary resuscitation (CPR) quality and optimize blood flow during CPR. Numerous factors impact EtCO2 (e.g., ventilation, metabolism, cardiac output), yet few clinical studies have correlated CPR quality and EtCO2 during actual out-of-hospital cardiac arrest (OHCA) resuscitations. The purpose of this study was to describe the association between EtCO2 and CPR quality variables during OHCA.
Methods: This is an observational study of prospectively collected CPR quality and capnography data from two EMS agencies participating in a statewide resuscitation quality improvement program. CPR quality and capnography data from adult (≥18 years) cardiac resuscitation attempts (10/2008–06/2013) were collected and analyzed on a minute-by-minute basis using RescueNet™ Code Review. Linear mixed effect models were used to evaluate the association between (log-transformed) EtCO2 level and CPR variables: chest compression (CC) depth, CC rate, CC release velocity (CCRV), ventilation rate.
Results: Among the 1217 adult OHCA cases of presumed cardiac etiology, 925 (76.0%) had a monitor-defibrillator file with CPR quality data, of which 296 (32.0%) cases had >1 minute of capnography data during CPR. After capnography quality review, 66 of these cases (22.3%) were excluded due to uninterpretable capnography, resulting in a final study sample of 230 subjects (mean age 68 years; 69.1% male), with a total of 1581 minutes of data. After adjustment for other CPR variables, a 10 mm increase in CC depth was associated with a 4.0% increase in EtCO2 (p < 0.0001), a 10 compression/minute increase in CC rate with a 1.7% increase in EtCO2 (p = 0.02), a 10 mm/second increase in CCRV with a 2.8% increase in EtCO2 (p = 0.03), and a 10 breath/minute increase in ventilation rate with a 17.4% decrease in EtCO2 (p < 0.0001).
Conclusion:When controlling for known CPR quality variables, increases in CC depth, CC rate and CCRV were each associated with a statistically significant but clinically modest increase in EtCO2. Given the small effect sizes, the clinical utility of using EtCO2 to guide CPR performance is unclear. Further research is needed to determine the practicality and impact of using real-time EtCO2 to guide CPR delivery in the prehospital environment.
ARAN Comment: There are clinically significant improvement in EtCO2 with increases in rate and depth of compressions. There are also other benefits, such as improvements in inter-thoracic pressure change i.e. improved aortic flow and TV through passive oxygenation. Minimal depths and rates should not be acceptable anymore as "competence" in effective resuscitation (particularly in adults).
Machine learning as a supportive tool to recognize cardiac arrest in emergency calls
Stig Nikolaj Blomberg, Fredrik Folke, Annette Kjær Ersbøll, Helle Collatz Christensen, Christian Torp-Pedersen, Michael R Sayre, Catherine R Counts, Freddy K Lippert
Resuscitation 2019 January 18
BACKGROUND: Emergency medical dispatchers fail to identify approximately 25% of cases of out of hospital cardiac arrest, thus lose the opportunity to provide the caller instructions in cardiopulmonary resuscitation. We examined whether a machine learning framework could recognise out-of-hospital cardiac arrest from audio files of calls to the emergency medical dispatch center.
METHODS: For all incidents responded to by Emergency Medical Dispatch Center Copenhagen in 2014, the associated call was retrieved. A machine learning framework was trained to recognise cardiac arrest from the recorded calls. Sensitivity, specificity, and positive predictive value for recognising out-of-hospital cardiac arrest were calculated. The performance of the machine learning framework was compared to the actual recognition and time-to-recognition of cardiac arrest by medical dispatchers.
RESULTS: We examined 108,607 emergency calls, of which 918 (0.8%) were out-of-hospital cardiac arrest calls eligible for analysis. Compared with medical dispatchers, the machine learning framework had a significantly higher sensitivity (72.5% vs. 84.1%, p < 0.001) with lower specificity (98.8% vs. 97.3%, p < 0.001). The machine learning framework had a lower positive predictive value than dispatchers (20.9% vs. 33.0%, p < 0.001). Time-to-recognition was significantly shorter for the machine learning framework compared to the dispatchers (median 44 seconds vs. 54 seconds, p < 0.001).
CONCLUSIONS: A machine learning framework performed better than emergency medical dispatchers for identifying out-of-hospital cardiac arrest in emergency phone calls. Machine learning may play an important role as a decision support tool for emergency medical dispatchers.
ARAN Comment: The use of a machine learning framework in future triage of calls is and interesting development (particularly for non-clinical emergency call-takers), however binary decision-making methodologies always assume the worst case scenario and therefore can disproportionately be "resource heavy" in responding to the "just in case scenario". Additionally a deceased patient and a cardiac arrest may elicit the same response, that a human operator may distinguish in the additional 10 seconds.
The effect of dispatcher-assisted cardiopulmonary resuscitation on early defibrillation and return of spontaneous circulation with survival
Sun Young Lee, Ki Jeong Hong, Sang Do Shin, Young Sun Ro, Kyoung Jun Song, Jeong Ho Park, So Yeon Kong, Tae Han Kim, Seung Chul Lee.
Resuscitation 2019 January 9
BACKGROUND: Dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) programs are implemented to augment bystander CPR and improve outcomes of patients with out-of-hospital cardiac arrest (OHCA). To understand the pathway of how DA-CPR improves outcomes of OHCA, we aimed to evaluate the effect of DA-CPR on defibrillation and return of spontaneous circulation (ROSC) with survival to hospital discharge within 90 minutes.
METHODS: We conducted a population-based observational study of all adults with OHCA with presumed cardiac aetiology treated by emergency medical services (EMS) between 2013 and 2016, using a national OHCA registry. We excluded cases without a witness, those that occurred in hospital, were witnessed by an EMS provider, or defibrillated by a layperson. The exposure was bystander CPR status: no bystander CPR (No BCPR), bystander CPR without dispatcher assistance (NDA-BCPR), and bystander CPR with dispatcher assistance (DA-BCPR). The observation time was set to a maximum of 90 minutes for survival analysis. The primary outcome was ROSC within 90 minutes leading to being discharged alive (ROSC with survival). The secondary outcomes were ROSC within 90 minutes leading to being discharged with cerebral performance category I or II (ROSC with good CPC) and first defibrillation within 90 minutes (defibrillation). Multivariable Cox proportional hazards analysis was performed to calculate adjusted hazard ratios (AHRs), according to bystander CPR status adjusted for potential confounders.
RESULTS: Of 25,450 eligible OHCAs, NDA-BCPR was provided for 3,193 cases (12.5%) and DA-BCPR was provided for 12,154 cases (47.8%). ROSC with survival was observed in 13.2% of cases with NDA-BCPR and 12.0% with DA-BCPR. Compared with No BCPR, both type of bystander CPR were associated with 44% and 55% increases in ROSC with survival to discharge (AHR, 95% confidence interval (CI): 1.44, 1.27 to 1.63 for NDA-BCPR and 1.55, 1.41 to 1.69 for DA-BCPR). DA-BCPR was also associated with defibrillation compared with No-BCPR, accounting for ROSC as a competing risk (AHR 1.16, 95% CI 1.12 to 1.21).
CONCLUSIONS: Compared with no bystander CPR provided, both bystander CPR with or without dispatcher assistance were associated with defibrillation and ROSC leading to survival to discharge in patients with witnessed OHCA.
ARAN Comment: Con-founders in this and other studies include the early recognition of OHCA by emergency operators and the nature of the instructions given i.e. compressions only vs. traditional CPR.
Sun Young Lee, Ki Jeong Hong, Sang Do Shin, Young Sun Ro, Kyoung Jun Song, Jeong Ho Park, So Yeon Kong, Tae Han Kim, Seung Chul Lee.
Resuscitation 2019 January 9
BACKGROUND: Dispatcher-assisted cardiopulmonary resuscitation (DA-CPR) programs are implemented to augment bystander CPR and improve outcomes of patients with out-of-hospital cardiac arrest (OHCA). To understand the pathway of how DA-CPR improves outcomes of OHCA, we aimed to evaluate the effect of DA-CPR on defibrillation and return of spontaneous circulation (ROSC) with survival to hospital discharge within 90 minutes.
METHODS: We conducted a population-based observational study of all adults with OHCA with presumed cardiac aetiology treated by emergency medical services (EMS) between 2013 and 2016, using a national OHCA registry. We excluded cases without a witness, those that occurred in hospital, were witnessed by an EMS provider, or defibrillated by a layperson. The exposure was bystander CPR status: no bystander CPR (No BCPR), bystander CPR without dispatcher assistance (NDA-BCPR), and bystander CPR with dispatcher assistance (DA-BCPR). The observation time was set to a maximum of 90 minutes for survival analysis. The primary outcome was ROSC within 90 minutes leading to being discharged alive (ROSC with survival). The secondary outcomes were ROSC within 90 minutes leading to being discharged with cerebral performance category I or II (ROSC with good CPC) and first defibrillation within 90 minutes (defibrillation). Multivariable Cox proportional hazards analysis was performed to calculate adjusted hazard ratios (AHRs), according to bystander CPR status adjusted for potential confounders.
RESULTS: Of 25,450 eligible OHCAs, NDA-BCPR was provided for 3,193 cases (12.5%) and DA-BCPR was provided for 12,154 cases (47.8%). ROSC with survival was observed in 13.2% of cases with NDA-BCPR and 12.0% with DA-BCPR. Compared with No BCPR, both type of bystander CPR were associated with 44% and 55% increases in ROSC with survival to discharge (AHR, 95% confidence interval (CI): 1.44, 1.27 to 1.63 for NDA-BCPR and 1.55, 1.41 to 1.69 for DA-BCPR). DA-BCPR was also associated with defibrillation compared with No-BCPR, accounting for ROSC as a competing risk (AHR 1.16, 95% CI 1.12 to 1.21).
CONCLUSIONS: Compared with no bystander CPR provided, both bystander CPR with or without dispatcher assistance were associated with defibrillation and ROSC leading to survival to discharge in patients with witnessed OHCA.
ARAN Comment: Con-founders in this and other studies include the early recognition of OHCA by emergency operators and the nature of the instructions given i.e. compressions only vs. traditional CPR.
Cardiopulmonary resuscitation performed by off-duty medical professionals versus laypersons and survival from out-of-hospital cardiac arrest among adult patients
Daisuke Kobayashi, Tetsuhisa Kitamura, Kosuke Kiyohara, Chika Nishiyama, Sumito Hayashida, Tasuku Matsuyama, Yusuke Katayama, Tomonari Shimamoto, Takeyuki Kiguchi, Satoe Okabayashi, Takashi Kawamura, Taku Iwami
Resuscitation 2019 January 9
BACKGROUND: Cardiopulmonary resuscitation (CPR) performed by bystanders is a key factor for out-of-hospital cardiac arrest (OHCA) survival. This study aimed to evaluate the relationship between CPR performed by off-duty medical professionals vs. laypersons and one-month survival with favorable neurological outcome after OHCA.
METHODS: Using a population-based database of OHCA patients in Osaka City, Japan, from 2013 through 2015, we enrolled adult OHCA patients with resuscitation attempts performed by bystanders before the arrival of emergency-medical-service personnel. Multi-variable logistic regression analysis was performed to assess the association between CPR performed by off-duty medical professionals vs. laypersons and the OHCA outcome after adjusting for potential confounding factors. The primary outcome measure was one-month survival with favourable neurological outcome, defined as cerebral performance category of 1 or 2.
RESULTS: A total of 2,326 subjects were eligible for our study. Among these, 365 (15.7%) patients received CPR by off-duty medical professionals and 1,961 (84.3%) received CPR by laypersons. In the multi-variable analysis, there was no difference in favourable neurological outcome between off-duty medical professionals (6.3% [23/365]) and laypersons (5.1% [100/1,961]) among eligible patients (adjusted odds ratio 0.83, 95% confidence interval [0.37-2.06]). This finding was also confirmed in propensity score-matched patients.
CONCLUSIONS: In Japan where the CPR training or bystander CPR has been widely disseminating, CPR by laypersons had similar effects compared to that by off-duty medical professionals. As this study could not assess the quality of bystander CPR, further studies are essential to verify the effects of the bystander CPR type on OHCA patients.
ARAN Comment: There is a huge variance in medical professional competence and experience with cardiac arrest and many have only a BLS requirement. Additionally, without the resources of a medical facility (i.e hospital) the level of intervention (and thus impact) will be diminished. Without specific data on the type and quality of the resuscitation it is difficult to make any recommendations.
Daisuke Kobayashi, Tetsuhisa Kitamura, Kosuke Kiyohara, Chika Nishiyama, Sumito Hayashida, Tasuku Matsuyama, Yusuke Katayama, Tomonari Shimamoto, Takeyuki Kiguchi, Satoe Okabayashi, Takashi Kawamura, Taku Iwami
Resuscitation 2019 January 9
BACKGROUND: Cardiopulmonary resuscitation (CPR) performed by bystanders is a key factor for out-of-hospital cardiac arrest (OHCA) survival. This study aimed to evaluate the relationship between CPR performed by off-duty medical professionals vs. laypersons and one-month survival with favorable neurological outcome after OHCA.
METHODS: Using a population-based database of OHCA patients in Osaka City, Japan, from 2013 through 2015, we enrolled adult OHCA patients with resuscitation attempts performed by bystanders before the arrival of emergency-medical-service personnel. Multi-variable logistic regression analysis was performed to assess the association between CPR performed by off-duty medical professionals vs. laypersons and the OHCA outcome after adjusting for potential confounding factors. The primary outcome measure was one-month survival with favourable neurological outcome, defined as cerebral performance category of 1 or 2.
RESULTS: A total of 2,326 subjects were eligible for our study. Among these, 365 (15.7%) patients received CPR by off-duty medical professionals and 1,961 (84.3%) received CPR by laypersons. In the multi-variable analysis, there was no difference in favourable neurological outcome between off-duty medical professionals (6.3% [23/365]) and laypersons (5.1% [100/1,961]) among eligible patients (adjusted odds ratio 0.83, 95% confidence interval [0.37-2.06]). This finding was also confirmed in propensity score-matched patients.
CONCLUSIONS: In Japan where the CPR training or bystander CPR has been widely disseminating, CPR by laypersons had similar effects compared to that by off-duty medical professionals. As this study could not assess the quality of bystander CPR, further studies are essential to verify the effects of the bystander CPR type on OHCA patients.
ARAN Comment: There is a huge variance in medical professional competence and experience with cardiac arrest and many have only a BLS requirement. Additionally, without the resources of a medical facility (i.e hospital) the level of intervention (and thus impact) will be diminished. Without specific data on the type and quality of the resuscitation it is difficult to make any recommendations.
Community-Wide Dissemination of Bystander Cardiopulmonary Resuscitation and Automated External Defibrillator Use Using a 45-Minute Chest Compression-Only Cardiopulmonary Resuscitation Training
Chika Nishiyama, Tetsuhisa Kitamura, Tomohiko Sakai, Yukiko Murakami, Tomonari Shimamoto, Takashi Kawamura, Takahiro Yonezawa, Shohei Nakai, Seishiro Marukawa, Tetsuya Sakamoto, Taku Iwami
Journal of the American Heart Association 2019 January 8, 8 (1): e009436
Background: Little is known about whether cardiopulmonary resuscitation ( CPR ) training can increase bystander CPR in the community or the appropriate target number of CPR trainings. Herein, we aimed to demonstrate community-wide aggressive dissemination of CPR training and evaluate temporal trends in bystander CPR .
Methods and Results: We provided CPR training (45-minute chest compression-only CPR plus automated external defibrillator use training or the conventional CPR training), targeting 16% of residents. All emergency medical service-treated out-of-hospital cardiac arrests of medical origin were included. Data on patients experiencing out-of-hospital cardiac arrest and bystander CPR quality were prospectively collected from September 2010 to December 2015. The primary outcome was the proportion of high-quality bystander CPR . During the study period, 57 173 residents (14.7%) completed the chest compression-only CPR training and 32 423 (8.3%) completed conventional CPR training. The proportion of bystander CPR performed did not change (from 43.3% in 2010 to 42.0% in 2015; P for trend=0.915), but the proportion of high-quality bystander CPR delivery increased from 11.7% in 2010 to 20.7% in 2015 ( P for trend=0.015). The 1-year increment was associated with high-quality bystander CPR (adjusted odds ratio, 1.461; 95% CI, 1.055-2.024). Bystanders who previously experienced CPR training were 3.432 times (95% CI, 1.170-10.071) more likely to perform high-quality CPR than those who did not.
Conclusions: We trained 23.0% of the residents in the medium-sized city of Osaka, Japan, and demonstrated that the proportion of high-quality CPR performed on the scene increased gradually, whereas that of bystander CPR delivered overall remained stable.
ARAN Comment: It is unfortunate in Australia that there are political interests that want to keep CPR as formal training. It is also disappointing the outcomes from research such as this (about the benefit of compression-only training) will be disregarded by the ARC without appropriate consideration so as to perpetuate an historical view.
Chika Nishiyama, Tetsuhisa Kitamura, Tomohiko Sakai, Yukiko Murakami, Tomonari Shimamoto, Takashi Kawamura, Takahiro Yonezawa, Shohei Nakai, Seishiro Marukawa, Tetsuya Sakamoto, Taku Iwami
Journal of the American Heart Association 2019 January 8, 8 (1): e009436
Background: Little is known about whether cardiopulmonary resuscitation ( CPR ) training can increase bystander CPR in the community or the appropriate target number of CPR trainings. Herein, we aimed to demonstrate community-wide aggressive dissemination of CPR training and evaluate temporal trends in bystander CPR .
Methods and Results: We provided CPR training (45-minute chest compression-only CPR plus automated external defibrillator use training or the conventional CPR training), targeting 16% of residents. All emergency medical service-treated out-of-hospital cardiac arrests of medical origin were included. Data on patients experiencing out-of-hospital cardiac arrest and bystander CPR quality were prospectively collected from September 2010 to December 2015. The primary outcome was the proportion of high-quality bystander CPR . During the study period, 57 173 residents (14.7%) completed the chest compression-only CPR training and 32 423 (8.3%) completed conventional CPR training. The proportion of bystander CPR performed did not change (from 43.3% in 2010 to 42.0% in 2015; P for trend=0.915), but the proportion of high-quality bystander CPR delivery increased from 11.7% in 2010 to 20.7% in 2015 ( P for trend=0.015). The 1-year increment was associated with high-quality bystander CPR (adjusted odds ratio, 1.461; 95% CI, 1.055-2.024). Bystanders who previously experienced CPR training were 3.432 times (95% CI, 1.170-10.071) more likely to perform high-quality CPR than those who did not.
Conclusions: We trained 23.0% of the residents in the medium-sized city of Osaka, Japan, and demonstrated that the proportion of high-quality CPR performed on the scene increased gradually, whereas that of bystander CPR delivered overall remained stable.
ARAN Comment: It is unfortunate in Australia that there are political interests that want to keep CPR as formal training. It is also disappointing the outcomes from research such as this (about the benefit of compression-only training) will be disregarded by the ARC without appropriate consideration so as to perpetuate an historical view.
Ambulance Density and Outcomes After Out-of-Hospital Cardiac Arrest: Insights from the Paris- Sudden Death Expertise Centre Registry
Richard Chocron, Thomas Loeb, Lionel Lamhaut, Daniel Jost, Frédéric Adnet, Eric Lecarpentier, Wulfran Bougouin, Franckie Beganton, Philippe Juvin, Eloi Marijon, Xavier Jouven, Alain Cariou, Florence Dumas
Circulation 2018 December 4
BACKGROUND: In out-of-hospital cardiac arrest (OHCA), geographic disparities in outcomes may reflect baseline variations in patients' characteristics but may also result from differences in the number of ambulances providing basic life support (BLS) and advanced life support (ALS). We aimed at assessing the association between allocated ambulance resources and outcomes in OHCA patients in a large urban community.
METHODS: From May 2011 to January 2016, we analyzed a prospectively collected Utstein database for all OHCA adults. Cases were geocoded according to 19 neighbourhoods and the number of BLS (firefighters performing cardiopulmonary resuscitation and applying automated external defibrillator) and ALS ambulances (medicalized team providing advanced care such as drugs and endotracheal intubation) was collected. We assessed the respective associations of Utstein parameters, socio-economic characteristics and ambulance resources of these neighbourhoods using a mixed-effect model with successful return of spontaneous circulation (ROSC) as the primary endpoint and survival at hospital discharge as a secondary endpoint.
RESULTS: During the study period, 8754 non-traumatic OHCA occurred in the Greater Paris area. Overall ROSC rate was 3675/8754 (41.9%) and survival rate at hospital discharge was 788/8754 (9%), ranging from 33% to 51.1% and from 4.4% to 14.5 % respectively, according to neighbourhoods (p<0.001). Patient and socio-demographic characteristics significantly differed between neighbourhoods (p for trend< 0.001). After adjustment, a higher density of ambulances was associated with successful ROSC (respectively adjusted Odds-Ratio (aOR)=1.31 (1.14-1.51); p<0.001 for ALS ambulances >1.5 per neighbourhood and aOR=1.21 (1.04-1.41); p=0.01 for BLS ambulances >4 per neighbourhood). Regarding survival at discharge, only the number of ALS ambulances >1.5 per neighbourhood was significant (aOR= 1.30 (1.06-1.59) p=0.01).
CONCLUSIONS: In this large urban population-based study of out-of-hospital cardiac arrests patients, we observed that allocated resources of Emergency Medical Service (EMS) are associated with outcome, suggesting that improving healthcare organisation may attenuate disparities in prognosis.
ARAN Comment: Australia suffers from the two-edged sword of a dispersed population over a large geographical area (when compared to other countries) and low resourcing of Ambulance services. The significance of ALS ambulances reflects other research that indicated ALS if implemented after 6 minutes from the time of the arrest has minimal impact on survival to discharge i.e merely increases ROSC and survival to a health facility.
Richard Chocron, Thomas Loeb, Lionel Lamhaut, Daniel Jost, Frédéric Adnet, Eric Lecarpentier, Wulfran Bougouin, Franckie Beganton, Philippe Juvin, Eloi Marijon, Xavier Jouven, Alain Cariou, Florence Dumas
Circulation 2018 December 4
BACKGROUND: In out-of-hospital cardiac arrest (OHCA), geographic disparities in outcomes may reflect baseline variations in patients' characteristics but may also result from differences in the number of ambulances providing basic life support (BLS) and advanced life support (ALS). We aimed at assessing the association between allocated ambulance resources and outcomes in OHCA patients in a large urban community.
METHODS: From May 2011 to January 2016, we analyzed a prospectively collected Utstein database for all OHCA adults. Cases were geocoded according to 19 neighbourhoods and the number of BLS (firefighters performing cardiopulmonary resuscitation and applying automated external defibrillator) and ALS ambulances (medicalized team providing advanced care such as drugs and endotracheal intubation) was collected. We assessed the respective associations of Utstein parameters, socio-economic characteristics and ambulance resources of these neighbourhoods using a mixed-effect model with successful return of spontaneous circulation (ROSC) as the primary endpoint and survival at hospital discharge as a secondary endpoint.
RESULTS: During the study period, 8754 non-traumatic OHCA occurred in the Greater Paris area. Overall ROSC rate was 3675/8754 (41.9%) and survival rate at hospital discharge was 788/8754 (9%), ranging from 33% to 51.1% and from 4.4% to 14.5 % respectively, according to neighbourhoods (p<0.001). Patient and socio-demographic characteristics significantly differed between neighbourhoods (p for trend< 0.001). After adjustment, a higher density of ambulances was associated with successful ROSC (respectively adjusted Odds-Ratio (aOR)=1.31 (1.14-1.51); p<0.001 for ALS ambulances >1.5 per neighbourhood and aOR=1.21 (1.04-1.41); p=0.01 for BLS ambulances >4 per neighbourhood). Regarding survival at discharge, only the number of ALS ambulances >1.5 per neighbourhood was significant (aOR= 1.30 (1.06-1.59) p=0.01).
CONCLUSIONS: In this large urban population-based study of out-of-hospital cardiac arrests patients, we observed that allocated resources of Emergency Medical Service (EMS) are associated with outcome, suggesting that improving healthcare organisation may attenuate disparities in prognosis.
ARAN Comment: Australia suffers from the two-edged sword of a dispersed population over a large geographical area (when compared to other countries) and low resourcing of Ambulance services. The significance of ALS ambulances reflects other research that indicated ALS if implemented after 6 minutes from the time of the arrest has minimal impact on survival to discharge i.e merely increases ROSC and survival to a health facility.
Field termination-of-resuscitation rule for refractory out-of-hospital cardiac arrests in Japan
Yoshikazu Goto, Akira Funada, Tetsuo Maeda, Hirofumi Okada, Yumiko Goto
Journal of Cardiology 2018 December 20
BACKGROUND: Guidelines for cardiopulmonary resuscitation (CPR) recommend using the universal termination-of-resuscitation (TOR) rule to identify out-of-hospital cardiac arrest (OHCA) patients eligible for field termination of resuscitation, thus avoiding medically futile transportation to the hospital. However, in Japan, emergency medical services (EMS) personnel are forbidden from terminating CPR in the field and transport almost all patients with OHCA to hospitals. We aimed to develop and validate a novel TOR rule to identify patients eligible for field termination of CPR.
METHODS: We analyzed 540,478 patients with OHCA from 2011 to 2015 using a Japanese registry. Main outcome measures were specificity and positive predictive value (PPV) of the newly developed TOR rule in predicting 1-month mortality after OHCA.
RESULTS: Recursive partitioning analysis in the development group (n=434,208) showed that EMS personnel could consider TOR if patients with OHCA met all of the following five criteria: (1) initial asystole, (2) arrest unwitnessed by a bystander, (3) age ≥81 years, (4) no bystander-administered CPR or automated external defibrillator use before EMS arrival, and (5) no return of spontaneous circulation after EMS-initiated CPR for 14min. For patients meeting these criteria, specificity and PPV for predicting 1-month mortality were 99.2% [95% confidence interval (CI), 99.0-99.3%] and 99.7% (95% CI, 99.6-99.7%), respectively, for the development group and were 99.5% (95% CI, 99.3-99.7%) and 99.8% (95% CI, 99.7-99.9%), respectively, for the validation group. Implementation of this novel rule would reduce patient transports to hospitals by 10.6% in the development group and 10.4% in the validation group.
CONCLUSIONS: Having both high specificity and PPV of >99% for predicting 1-month mortality, our developed TOR rule may be applied in the field for Japanese patients with OHCA who meet all five criteria. Prospective validation studies and establishment of prehospital EMS protocol are required before implementing this rule.
ARAN Comment: This set of criteria for TOR in Japan goes some way toward more pragmatic responses to OHCA, however it still does not go far enough in reflecting the reality of survival (regardless of age) rather than assuming a incredibly small chance (despite the clear evidence about survival to discharge) is worth transportation (where treatment during transport is sub-optimal and in an ED no additional measures may be affected).
Yoshikazu Goto, Akira Funada, Tetsuo Maeda, Hirofumi Okada, Yumiko Goto
Journal of Cardiology 2018 December 20
BACKGROUND: Guidelines for cardiopulmonary resuscitation (CPR) recommend using the universal termination-of-resuscitation (TOR) rule to identify out-of-hospital cardiac arrest (OHCA) patients eligible for field termination of resuscitation, thus avoiding medically futile transportation to the hospital. However, in Japan, emergency medical services (EMS) personnel are forbidden from terminating CPR in the field and transport almost all patients with OHCA to hospitals. We aimed to develop and validate a novel TOR rule to identify patients eligible for field termination of CPR.
METHODS: We analyzed 540,478 patients with OHCA from 2011 to 2015 using a Japanese registry. Main outcome measures were specificity and positive predictive value (PPV) of the newly developed TOR rule in predicting 1-month mortality after OHCA.
RESULTS: Recursive partitioning analysis in the development group (n=434,208) showed that EMS personnel could consider TOR if patients with OHCA met all of the following five criteria: (1) initial asystole, (2) arrest unwitnessed by a bystander, (3) age ≥81 years, (4) no bystander-administered CPR or automated external defibrillator use before EMS arrival, and (5) no return of spontaneous circulation after EMS-initiated CPR for 14min. For patients meeting these criteria, specificity and PPV for predicting 1-month mortality were 99.2% [95% confidence interval (CI), 99.0-99.3%] and 99.7% (95% CI, 99.6-99.7%), respectively, for the development group and were 99.5% (95% CI, 99.3-99.7%) and 99.8% (95% CI, 99.7-99.9%), respectively, for the validation group. Implementation of this novel rule would reduce patient transports to hospitals by 10.6% in the development group and 10.4% in the validation group.
CONCLUSIONS: Having both high specificity and PPV of >99% for predicting 1-month mortality, our developed TOR rule may be applied in the field for Japanese patients with OHCA who meet all five criteria. Prospective validation studies and establishment of prehospital EMS protocol are required before implementing this rule.
ARAN Comment: This set of criteria for TOR in Japan goes some way toward more pragmatic responses to OHCA, however it still does not go far enough in reflecting the reality of survival (regardless of age) rather than assuming a incredibly small chance (despite the clear evidence about survival to discharge) is worth transportation (where treatment during transport is sub-optimal and in an ED no additional measures may be affected).
Optimal Scene Time to Achieve Favourable Outcomes in Out-of-hospital Cardiac Arrest: How Long Is Too Long?
Glenn Goodwin, Dyana Picache, Brian J Louie, Nicholas Gaeto, Tarik Zeid, Paxton P Aung, Armando Clift, Sonu Sahni
Curēus 2018 October 9, 10 (10): e3434
Background: Despite advances in resuscitation science and public health, out-of-hospital cardiac arrest (OOHCA) cases have an average survival rate of only 12% nationwide, compared to 24.8% of cases occurring in hospital. Many factors, including resuscitation interventions, contribute to positive patient outcomes and have, therefore, been studied in attempts to optimise emergency medical services (EMS) protocols to achieve higher rates of return of spontaneous circulation (ROSC) in the field. However, no consensus has been met regarding the appropriate amount of time for EMS to spend on scene. Aim A favourable outcome is defined as patients that achieved the combination of ROSC and a final disposition of "ongoing resuscitation in the emergency department (ED)." The primary purpose of this preliminary study was to determine the scene time interval (STI) in which American urban EMS systems achieved the highest rates of favourable outcomes in non-traumatic OOHCAs.
Methods: All EMS-related data, including demographics, presenting rhythm, airway management, chemical interventions, and ROSC were recorded using a standardised EMS charting system by the highest-ranking EMS provider on the ambulance. The reports were retrospectively collected and analysed.
Conclusion: Our data suggest that the optimal 20-minute STI for OOHCA patients in an urban EMS system is between 41 and 60 minutes. Interestingly, the 10-minute interval within the 41-60 minute cohort that provided the highest rate of ROSC was between 41 and 50 minutes. Generally, the longer the STI, the greater the percentage of favourable outcomes up to the 50-minute mark. Once past 50 minutes, a phenomenon of diminishing return was observed and the rates of favourable outcomes sharply declined. This suggests a possible "sweet spot" that may exist regarding the optimal scene time in a cardiac arrest encounter. Significant differences between the average number of interventions per patient were found, however, many confounding factors and the limited data set make the results difficult to generalise.
ARAN Comment: Many of these studies into scene time have too many variables to make any recommendation on scene time. The variables of most concern are differences in the level of care provided on scene and the definition of a "favourable outcome" (as this can merely be a ROSC in deference to survival to discharge, without significant cerebral deficit). The studies also tend to assume that "definitive care" is only available in a hospital, as is the capacity to determine TOR.
Glenn Goodwin, Dyana Picache, Brian J Louie, Nicholas Gaeto, Tarik Zeid, Paxton P Aung, Armando Clift, Sonu Sahni
Curēus 2018 October 9, 10 (10): e3434
Background: Despite advances in resuscitation science and public health, out-of-hospital cardiac arrest (OOHCA) cases have an average survival rate of only 12% nationwide, compared to 24.8% of cases occurring in hospital. Many factors, including resuscitation interventions, contribute to positive patient outcomes and have, therefore, been studied in attempts to optimise emergency medical services (EMS) protocols to achieve higher rates of return of spontaneous circulation (ROSC) in the field. However, no consensus has been met regarding the appropriate amount of time for EMS to spend on scene. Aim A favourable outcome is defined as patients that achieved the combination of ROSC and a final disposition of "ongoing resuscitation in the emergency department (ED)." The primary purpose of this preliminary study was to determine the scene time interval (STI) in which American urban EMS systems achieved the highest rates of favourable outcomes in non-traumatic OOHCAs.
Methods: All EMS-related data, including demographics, presenting rhythm, airway management, chemical interventions, and ROSC were recorded using a standardised EMS charting system by the highest-ranking EMS provider on the ambulance. The reports were retrospectively collected and analysed.
Conclusion: Our data suggest that the optimal 20-minute STI for OOHCA patients in an urban EMS system is between 41 and 60 minutes. Interestingly, the 10-minute interval within the 41-60 minute cohort that provided the highest rate of ROSC was between 41 and 50 minutes. Generally, the longer the STI, the greater the percentage of favourable outcomes up to the 50-minute mark. Once past 50 minutes, a phenomenon of diminishing return was observed and the rates of favourable outcomes sharply declined. This suggests a possible "sweet spot" that may exist regarding the optimal scene time in a cardiac arrest encounter. Significant differences between the average number of interventions per patient were found, however, many confounding factors and the limited data set make the results difficult to generalise.
ARAN Comment: Many of these studies into scene time have too many variables to make any recommendation on scene time. The variables of most concern are differences in the level of care provided on scene and the definition of a "favourable outcome" (as this can merely be a ROSC in deference to survival to discharge, without significant cerebral deficit). The studies also tend to assume that "definitive care" is only available in a hospital, as is the capacity to determine TOR.
Effect of National Implementation of Telephone CPR Program to Improve Outcomes from Out-of-Hospital Cardiac Arrest: an Interrupted Time-Series Analysis
Yu Jin Lee, Seung-Sik Hwang, Sang Do Shin, Seung Chul Lee, Kyoung Jun Song
Journal of Korean Medical Science 2018 December 17, 33 (51): e328
Background: In cardiac arrest, the survival rate increases with the provision of bystander cardiopulmonary resuscitation (CPR), of which the initial response and treatment are critical. Telephone CPR is among the effective methods that might increase the provision of bystander CPR. This study aimed to describe and examine the improvement of neurological outcomes in individuals with out-of-hospital acute cardiac arrest by implementing the nationwide, standardised telephone CPR program.
Methods: Data from the emergency medical service-based cardiac arrest registry that were collected between 2009 and 2014 were used. The effectiveness of the intervention in the interrupted time-series study was determined via a segmented regression analysis, which showed the risk ratio and risk difference in good neurological outcomes before and after the intervention.
Results: Of 164,221 patients, 148,403 were analysed. However, patients with unknown sex and limited data on treatment outcomes were excluded. Approximately 64.3% patients were men, with an average age of 63.7 years. The number of bystander CPR increased by 3.3 times (95% confidence interval [CI], 3.1-3.5) after the intervention, whereas the rate of good neurological outcomes increased by 2.6 times (95% CI, 2.3-2.9 [1.6%]; 1.4-1.7). The excess number was identified based on the differences between the observed and predicted trends. In total, 2,127 cases of out-of-hospital cardiac arrest (OHCA) after the intervention period received additional bystander CPR, and 339 cases of OHCA had good neurological outcomes.
Conclusion: The nationwide implementation of the standardised telephone CPR program increased the number of bystander CPR and improved good neurological outcomes.
ARAN Comment: while it is encouraging to see other countries implementing and evaluating new initiatives to improve OHCA survival rates; it reinforces the lack of vision and innovation in Australia in this area. Unfortunately, continued trust and reliance on the ARC for improvement and innovation is misplaced and represents the biggest barrier to progress.
Yu Jin Lee, Seung-Sik Hwang, Sang Do Shin, Seung Chul Lee, Kyoung Jun Song
Journal of Korean Medical Science 2018 December 17, 33 (51): e328
Background: In cardiac arrest, the survival rate increases with the provision of bystander cardiopulmonary resuscitation (CPR), of which the initial response and treatment are critical. Telephone CPR is among the effective methods that might increase the provision of bystander CPR. This study aimed to describe and examine the improvement of neurological outcomes in individuals with out-of-hospital acute cardiac arrest by implementing the nationwide, standardised telephone CPR program.
Methods: Data from the emergency medical service-based cardiac arrest registry that were collected between 2009 and 2014 were used. The effectiveness of the intervention in the interrupted time-series study was determined via a segmented regression analysis, which showed the risk ratio and risk difference in good neurological outcomes before and after the intervention.
Results: Of 164,221 patients, 148,403 were analysed. However, patients with unknown sex and limited data on treatment outcomes were excluded. Approximately 64.3% patients were men, with an average age of 63.7 years. The number of bystander CPR increased by 3.3 times (95% confidence interval [CI], 3.1-3.5) after the intervention, whereas the rate of good neurological outcomes increased by 2.6 times (95% CI, 2.3-2.9 [1.6%]; 1.4-1.7). The excess number was identified based on the differences between the observed and predicted trends. In total, 2,127 cases of out-of-hospital cardiac arrest (OHCA) after the intervention period received additional bystander CPR, and 339 cases of OHCA had good neurological outcomes.
Conclusion: The nationwide implementation of the standardised telephone CPR program increased the number of bystander CPR and improved good neurological outcomes.
ARAN Comment: while it is encouraging to see other countries implementing and evaluating new initiatives to improve OHCA survival rates; it reinforces the lack of vision and innovation in Australia in this area. Unfortunately, continued trust and reliance on the ARC for improvement and innovation is misplaced and represents the biggest barrier to progress.
[Effects between chest-compression-only cardiopulmonary resuscitation and standard cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest: a Meta-analysis]
Xueli Liao, Bihua Chen, Hui Tang, Yanze Wang, Min Wang, Manhong Zhou
Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2018, 30 (11): 1017-1023
OBJECTIVE: To comprehensively evaluate and compare the resuscitation efficacy of chest-compression-only cardiopulmonary resuscitation (CCPR) and standard cardiopulmonary resuscitation (SCPR) for patients with out-of-hospital cardiac arrest (OHCA).
METHODS: Databases such as PubMed, Embase, Ovid, Cochrane Library, Wanfang, CNKI, VIP, CBM were searched from the date of their foundation to March 2nd 2018, and the studies on the difference of effects between CCPR and SCPR for patients with OHCA were retrieved. The outcomes included the return of spontaneous circulation (ROSC) rate, survival to hospital discharge, neurological function completion rate. Two reviewers independently screened the literature meeting the inclusion criteria, independently collected information and evaluated the literature quality. Meta-analysis was conducted using RevMan 5.3 software, and sensitivity analysis was conducted by selecting model analysis method and removing single research method. Funnel plot was used to evaluate publication bias.
RESULTS: A total of 10 cohort studies were included, including 174 163 patients with OHCA, of which 95 157 undergone CCPR and 79 006 undergone SCPR. The scores of the Newcastle-Ottawa scale (NOS) were 8-9, indicating that the quality of the literatures included was high. It was shown by the Meta-analysis that CCPR had the higher rate of survival to hospital discharge [relative risk (RR) = 1.04, 95% confidence interval (95%CI) = 1.00-1.08, P = 0.04] and neurological function completion (RR = 1.11, 95%CI = 1.06-1.17, P < 0.000 1) than SCPR, but there was no significant difference in ROSC rate between the two groups (RR = 1.01, 95%CI = 0.98-1.04, P = 0.52). In the subgroup, there was no statistical significance between CCPR and SCPR in the rate of survival to hospital discharge in cardiac OHCA patients (RR = 1.13, 95%CI = 0.82-1.57, P = 0.45). However, in non-cardiac OHCA group, SCPR showed more benefits than CCPR in improving the rate of survival to hospital discharge (RR = 0.88, 95%CI = 0.80-0.96, P = 0.004). The above analysis results were consistent in the fixed effect model and random effect model, indicating that the results were reliable and stable. It was shown by the funnel plot that most of the studies were left-right inverted funnel type, indicating a low publication bias. However, the bias could not be completely excluded due to the small number of included literatures.
CONCLUSIONS: For patients without OHCA etiological classification, CCPR was not less than SCPR in improving ROSC rate, discharge survival rate and good neurological function, and CCPR was more advantageous in learning and the willingness of bystanders to implement. However, when non-cardiogenic OHCA could be identified, SCPR should be recommended when conditions permit.
ARAN Comment: The message is clear to everyone (except Australia and NZ who refuse to listen); in SCA CCPR should be the default and SCPR for other causes.
Xueli Liao, Bihua Chen, Hui Tang, Yanze Wang, Min Wang, Manhong Zhou
Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2018, 30 (11): 1017-1023
OBJECTIVE: To comprehensively evaluate and compare the resuscitation efficacy of chest-compression-only cardiopulmonary resuscitation (CCPR) and standard cardiopulmonary resuscitation (SCPR) for patients with out-of-hospital cardiac arrest (OHCA).
METHODS: Databases such as PubMed, Embase, Ovid, Cochrane Library, Wanfang, CNKI, VIP, CBM were searched from the date of their foundation to March 2nd 2018, and the studies on the difference of effects between CCPR and SCPR for patients with OHCA were retrieved. The outcomes included the return of spontaneous circulation (ROSC) rate, survival to hospital discharge, neurological function completion rate. Two reviewers independently screened the literature meeting the inclusion criteria, independently collected information and evaluated the literature quality. Meta-analysis was conducted using RevMan 5.3 software, and sensitivity analysis was conducted by selecting model analysis method and removing single research method. Funnel plot was used to evaluate publication bias.
RESULTS: A total of 10 cohort studies were included, including 174 163 patients with OHCA, of which 95 157 undergone CCPR and 79 006 undergone SCPR. The scores of the Newcastle-Ottawa scale (NOS) were 8-9, indicating that the quality of the literatures included was high. It was shown by the Meta-analysis that CCPR had the higher rate of survival to hospital discharge [relative risk (RR) = 1.04, 95% confidence interval (95%CI) = 1.00-1.08, P = 0.04] and neurological function completion (RR = 1.11, 95%CI = 1.06-1.17, P < 0.000 1) than SCPR, but there was no significant difference in ROSC rate between the two groups (RR = 1.01, 95%CI = 0.98-1.04, P = 0.52). In the subgroup, there was no statistical significance between CCPR and SCPR in the rate of survival to hospital discharge in cardiac OHCA patients (RR = 1.13, 95%CI = 0.82-1.57, P = 0.45). However, in non-cardiac OHCA group, SCPR showed more benefits than CCPR in improving the rate of survival to hospital discharge (RR = 0.88, 95%CI = 0.80-0.96, P = 0.004). The above analysis results were consistent in the fixed effect model and random effect model, indicating that the results were reliable and stable. It was shown by the funnel plot that most of the studies were left-right inverted funnel type, indicating a low publication bias. However, the bias could not be completely excluded due to the small number of included literatures.
CONCLUSIONS: For patients without OHCA etiological classification, CCPR was not less than SCPR in improving ROSC rate, discharge survival rate and good neurological function, and CCPR was more advantageous in learning and the willingness of bystanders to implement. However, when non-cardiogenic OHCA could be identified, SCPR should be recommended when conditions permit.
ARAN Comment: The message is clear to everyone (except Australia and NZ who refuse to listen); in SCA CCPR should be the default and SCPR for other causes.
The American Heart Association announced that Texas Tech University Health Sciences Center is the official sponsor of a hands-only CPR training kiosk unveiled during a ribbon cutting event Tuesday morning at Lubbock Preston Smith International Airport.
The kiosk sits at the Lubbock Preston Smith International Airport between Gate 6 and Gate 7 to the left of security, where thousands of people visit each year, according to a statement from the Heart Association.
It features a touch screen with a video program that provides a brief introduction and overview of Hands-Only CPR, followed by a practice session and a 30-second test session. With the help of a practice manikin, or a rubber torso, the kiosk gives feedback about the depth and rate of compressions and proper hand placement – factors that influence the effectiveness of CPR. Organisers say the entire training takes about five minutes.
The Heart Association states the training opportunity will be helpful because, every year, more than 350,000 cardiac arrests occur outside of the hospital and more than 20 percent occur in public places like airports, casinos and sporting facilities. The Hands-Only CPR education available at each kiosk is designed to help users understand how they can immediately help a person who experiences a cardiac emergency outside of a hospital.
“Cardiac arrest remains a leading cause of death in the United States, and survival depends on immediately receiving CPR from someone nearby,” Dr. Scott Shurmur, M.D., a cardiologist at the Texas Tech Physicians – Center for Cardiovascular Health, said in a statement. “Although in-person training is still the best way to learn the skills necessary for high-quality CPR, the kiosk will provide additional training that could make a difference and save the life of someone you love.”
Kim Walker, a Heart Association volunteer and advocate, said about 90 percent of cardiac arrest victims die, often because bystanders don’t know how to start CPR or are afraid they’ll do something wrong.
“Bystander CPR, especially if administered immediately, can double or triple a cardiac arrest victim’s chance of survival, which is why the Hands-Only CPR education available at the kiosk is so valuable,” she said. “In just a matter of a few minutes, people will learn a skill that can potentially make a difference in the lives of those they love most as well as others.”
The two simple steps of Hands-Only CPR are: if a bystander sees a teen or adult collapse, he or she should first call 9-1-1. Then push hard and fast in the centre of the chest to the beat of “Stayin’ Alive,” which has 100 beats per minute (bpm). The Bee Gees’ song has the minimum rate you should push on the chest during Hands-Only CPR.
“The kiosks will help the community understand how simple it is to perform the two steps of Hands-Only CPR, which will hopefully help reduce some of the trepidation that people have about performing bystander CPR,” said Denise Sanders, senior corporate market director of the Heart Association in Lubbock. “After completing the kiosk training, we hope people will feel empowered knowing they are taking the first steps in learning a critical skill.”
ARAN Comment: Of course in Australia efforts to introduce similar kiosks have been undermined by our "authority" because it is "heresy" to consider teaching compressions without ventilations.
The kiosk sits at the Lubbock Preston Smith International Airport between Gate 6 and Gate 7 to the left of security, where thousands of people visit each year, according to a statement from the Heart Association.
It features a touch screen with a video program that provides a brief introduction and overview of Hands-Only CPR, followed by a practice session and a 30-second test session. With the help of a practice manikin, or a rubber torso, the kiosk gives feedback about the depth and rate of compressions and proper hand placement – factors that influence the effectiveness of CPR. Organisers say the entire training takes about five minutes.
The Heart Association states the training opportunity will be helpful because, every year, more than 350,000 cardiac arrests occur outside of the hospital and more than 20 percent occur in public places like airports, casinos and sporting facilities. The Hands-Only CPR education available at each kiosk is designed to help users understand how they can immediately help a person who experiences a cardiac emergency outside of a hospital.
“Cardiac arrest remains a leading cause of death in the United States, and survival depends on immediately receiving CPR from someone nearby,” Dr. Scott Shurmur, M.D., a cardiologist at the Texas Tech Physicians – Center for Cardiovascular Health, said in a statement. “Although in-person training is still the best way to learn the skills necessary for high-quality CPR, the kiosk will provide additional training that could make a difference and save the life of someone you love.”
Kim Walker, a Heart Association volunteer and advocate, said about 90 percent of cardiac arrest victims die, often because bystanders don’t know how to start CPR or are afraid they’ll do something wrong.
“Bystander CPR, especially if administered immediately, can double or triple a cardiac arrest victim’s chance of survival, which is why the Hands-Only CPR education available at the kiosk is so valuable,” she said. “In just a matter of a few minutes, people will learn a skill that can potentially make a difference in the lives of those they love most as well as others.”
The two simple steps of Hands-Only CPR are: if a bystander sees a teen or adult collapse, he or she should first call 9-1-1. Then push hard and fast in the centre of the chest to the beat of “Stayin’ Alive,” which has 100 beats per minute (bpm). The Bee Gees’ song has the minimum rate you should push on the chest during Hands-Only CPR.
“The kiosks will help the community understand how simple it is to perform the two steps of Hands-Only CPR, which will hopefully help reduce some of the trepidation that people have about performing bystander CPR,” said Denise Sanders, senior corporate market director of the Heart Association in Lubbock. “After completing the kiosk training, we hope people will feel empowered knowing they are taking the first steps in learning a critical skill.”
ARAN Comment: Of course in Australia efforts to introduce similar kiosks have been undermined by our "authority" because it is "heresy" to consider teaching compressions without ventilations.
Any bystander CPR is better than no CPR attempt - An Urban Myth, Misconception, or Proved Truth?
Zlatko Fischer, Violetta Raffay, Michael Buda, Nela Đorđević Vujovic, Ivana Obradović; Journal Resuscitatio Balcanica 2018; 11: 126-130
We have all heard it before (and seen it blazoned across a familiar home page) but many of us have seen the standard of resuscitation that bystanders are capable of and the guidelines they try to follow that just tend complicate and delay the implementation of essential treatment. Researchers in Serbia have studied the assumption of any CPR being better than none and found some disturbing (but not unsurprising results). To paraphrase the findings...
"According the majority opinion, “any CPR is better that no CPR” should be critically analysed. There are reasons to more deeply and carefully investigate the usefulness of bystander CPR. Our results indicate the this might even be harmful (i.e. politically correct rather than contributing to better outcomes). It was found in a study over 3 years involving over 4000 cardiac arrest, that a victim has a 1.6 times greater chance of a ROSC if there is no bystander CPR attempt. The chances of getting CPR increased by 2.8 times if there was a bystander present."
ARAN has been sceptical of this simplistic message and the genuineness of those who spruik it, for many years. Studies (and our own research) have shown that not only are effective (i.e. beneficial) compressions) applied by a minority of bystanders (trained or not), but that current BLS protocols that still emphasise ventilations in all arrests are detrimental in the pre-ambulance period for the majority of arrests (i.e. SCA 85%).
Zlatko Fischer, Violetta Raffay, Michael Buda, Nela Đorđević Vujovic, Ivana Obradović; Journal Resuscitatio Balcanica 2018; 11: 126-130
We have all heard it before (and seen it blazoned across a familiar home page) but many of us have seen the standard of resuscitation that bystanders are capable of and the guidelines they try to follow that just tend complicate and delay the implementation of essential treatment. Researchers in Serbia have studied the assumption of any CPR being better than none and found some disturbing (but not unsurprising results). To paraphrase the findings...
"According the majority opinion, “any CPR is better that no CPR” should be critically analysed. There are reasons to more deeply and carefully investigate the usefulness of bystander CPR. Our results indicate the this might even be harmful (i.e. politically correct rather than contributing to better outcomes). It was found in a study over 3 years involving over 4000 cardiac arrest, that a victim has a 1.6 times greater chance of a ROSC if there is no bystander CPR attempt. The chances of getting CPR increased by 2.8 times if there was a bystander present."
ARAN has been sceptical of this simplistic message and the genuineness of those who spruik it, for many years. Studies (and our own research) have shown that not only are effective (i.e. beneficial) compressions) applied by a minority of bystanders (trained or not), but that current BLS protocols that still emphasise ventilations in all arrests are detrimental in the pre-ambulance period for the majority of arrests (i.e. SCA 85%).
Association between chest compression rates and clinical outcomes following in-hospital cardiac arrest at an academic tertiary hospital
Author panel: J.HopeKilgannonaMichaelKirchhoffaLisaPiercebNicholasAunchmanaStephenTrzeciakabBrian W.Robertsa
https://doi.org/10.1016/j.resuscitation.2016.09.015
Abstract
Aims
Recent guidelines for management of cardiac arrest recommend chest compression rates of 100–120 compressions/min. However, animal studies have found cardiac output to increase with rates up to 150 compressions/min. The objective of this study was to test the association between chest compression rates during cardiopulmonary resuscitation for in-hospital cardiac arrest (IHCA) and outcome.
Methods
We conducted a prospective observational study at a single academic medical center. Inclusion criteria: age ≥ 18, IHCA, cardiopulmonary resuscitation performed. We analyzed chest compression rates measured by defibrillation electrodes, which recorded changes in thoracic impedance. The primary outcome was return of spontaneous circulation (ROSC). We used multivariable logistic regression to determine odds ratios for ROSC by chest compression rate categories (100–120, 121–140, >140 compressions/min), adjusted for chest compression fraction (proportion of time chest compressions provided) and other known predictors of outcome. We set 100–120 compressions/min as the reference category for the multivariable model.
Results
We enrolled 222 consecutive patients and found a mean chest compression rate of 139 ± 15. Overall 53% achieved ROSC; among 100–120, 121–140, and >140 compressions/min, ROSC was 29%, 64%, and 49% respectively. A chest compression rate of 121–140 compressions/min had the greatest likelihood of ROSC, odds ratio 4.48 (95% CI 1.42–14.14).
Conclusions
In this sample of adult IHCA patients, a chest compression rate of 121–140 compressions/min had the highest odds ratio of ROSC. Rates above the currently recommended 100–120 compressions/min may improve the chances of ROSC among IHCA patients.
Author panel: J.HopeKilgannonaMichaelKirchhoffaLisaPiercebNicholasAunchmanaStephenTrzeciakabBrian W.Robertsa
https://doi.org/10.1016/j.resuscitation.2016.09.015
Abstract
Aims
Recent guidelines for management of cardiac arrest recommend chest compression rates of 100–120 compressions/min. However, animal studies have found cardiac output to increase with rates up to 150 compressions/min. The objective of this study was to test the association between chest compression rates during cardiopulmonary resuscitation for in-hospital cardiac arrest (IHCA) and outcome.
Methods
We conducted a prospective observational study at a single academic medical center. Inclusion criteria: age ≥ 18, IHCA, cardiopulmonary resuscitation performed. We analyzed chest compression rates measured by defibrillation electrodes, which recorded changes in thoracic impedance. The primary outcome was return of spontaneous circulation (ROSC). We used multivariable logistic regression to determine odds ratios for ROSC by chest compression rate categories (100–120, 121–140, >140 compressions/min), adjusted for chest compression fraction (proportion of time chest compressions provided) and other known predictors of outcome. We set 100–120 compressions/min as the reference category for the multivariable model.
Results
We enrolled 222 consecutive patients and found a mean chest compression rate of 139 ± 15. Overall 53% achieved ROSC; among 100–120, 121–140, and >140 compressions/min, ROSC was 29%, 64%, and 49% respectively. A chest compression rate of 121–140 compressions/min had the greatest likelihood of ROSC, odds ratio 4.48 (95% CI 1.42–14.14).
Conclusions
In this sample of adult IHCA patients, a chest compression rate of 121–140 compressions/min had the highest odds ratio of ROSC. Rates above the currently recommended 100–120 compressions/min may improve the chances of ROSC among IHCA patients.
Application of a Dual-Dispatch System for Out-of-Hospital Cardiac Arrest Patients: Will More Hands Save More Lives?
Jung Ho Kim, Hyun Wook Ryoo, Jong Yeon Kim, Jae Yun Ahn, Sungbae Moon, Dong Eun Lee, You Ho Mun
Journal of Korean Medical Science 2019 September 2, 34 (34): e141
BACKGROUND: Recovery after out-of-hospital cardiac arrest (OHCA) is difficult, and emergency medical services (EMS) systems apply various strategies to improve outcomes. Multi-dispatch is one means of providing high-quality cardiopulmonary resuscitation (CPR), but no definitive best-operation guidelines are available. We assessed the effects of a basic life support (BLS)-based dual-dispatch system for OHCA.
METHODS: This prospective observational study of 898 enrolled OHCA patients, conducted in Daegu, Korea from March 1, 2015 to June 30, 2016, involved patients > 18 years old with suspected cardiac etiology OHCA. In Daegu, EMS started a BLS-based dual-dispatch system in March 2015, for cases of cardiac arrest recognition by a dispatch center. We assessed the association between dual-dispatch and OHCA outcomes using multivariate logistic regressions. We also analyzed the effect of dual-dispatch according to the stratified on-scene time.
RESULTS: Of 898 OHCA patients (median, 69.0 years; 65.5% men), dual-dispatch was applied in 480 (53.5%) patients. There was no difference between the single-dispatch group (SDG) and the dual-dispatch group (DDG) in survival at discharge and neurological outcomes (survival discharge, P = 0.176; neurological outcomes, P = 0.345). In the case of less than 10 minutes of on-scene time, the adjusted odds ratio was 1.749 (95% confidence interval [CI], 0.490-6.246) for survival discharge and 6.058 (95% CI, 1.346-27.277) for favorable neurological outcomes in the DDG compared with the SDG.
CONCLUSION: Dual-dispatch was not associated with better OHCA outcomes for the entire study population, but showed favorable neurological outcomes when the on-scene time was less than 10 minutes.
ARAN Comment: An interesting outcome that is in line with other research, showing that just "any" intervention in the first 6-8 minutes has minimal impact on long-term survival.
Jung Ho Kim, Hyun Wook Ryoo, Jong Yeon Kim, Jae Yun Ahn, Sungbae Moon, Dong Eun Lee, You Ho Mun
Journal of Korean Medical Science 2019 September 2, 34 (34): e141
BACKGROUND: Recovery after out-of-hospital cardiac arrest (OHCA) is difficult, and emergency medical services (EMS) systems apply various strategies to improve outcomes. Multi-dispatch is one means of providing high-quality cardiopulmonary resuscitation (CPR), but no definitive best-operation guidelines are available. We assessed the effects of a basic life support (BLS)-based dual-dispatch system for OHCA.
METHODS: This prospective observational study of 898 enrolled OHCA patients, conducted in Daegu, Korea from March 1, 2015 to June 30, 2016, involved patients > 18 years old with suspected cardiac etiology OHCA. In Daegu, EMS started a BLS-based dual-dispatch system in March 2015, for cases of cardiac arrest recognition by a dispatch center. We assessed the association between dual-dispatch and OHCA outcomes using multivariate logistic regressions. We also analyzed the effect of dual-dispatch according to the stratified on-scene time.
RESULTS: Of 898 OHCA patients (median, 69.0 years; 65.5% men), dual-dispatch was applied in 480 (53.5%) patients. There was no difference between the single-dispatch group (SDG) and the dual-dispatch group (DDG) in survival at discharge and neurological outcomes (survival discharge, P = 0.176; neurological outcomes, P = 0.345). In the case of less than 10 minutes of on-scene time, the adjusted odds ratio was 1.749 (95% confidence interval [CI], 0.490-6.246) for survival discharge and 6.058 (95% CI, 1.346-27.277) for favorable neurological outcomes in the DDG compared with the SDG.
CONCLUSION: Dual-dispatch was not associated with better OHCA outcomes for the entire study population, but showed favorable neurological outcomes when the on-scene time was less than 10 minutes.
ARAN Comment: An interesting outcome that is in line with other research, showing that just "any" intervention in the first 6-8 minutes has minimal impact on long-term survival.
Breakthrough for ARAN and common sense.
NSW Health first to release a new message for the initial management of suspected cardiac arrest!
NSW Health first to release a new message for the initial management of suspected cardiac arrest!
After a lot of debate, lobbying and support from other groups passionate about improving cardiac arrest survival rates, NSW has changed its messaging to reflect world's best-practice for the initial response to suspected cardiac arrest. The traditional and largely redundant DRSABCD advice for the public has been replaced with a simple message that is supported by the international evidence: CALL-PUSH-SHOCK i.e. the only 3 things that have proven to improve cardiac arrest survival rates in Sudden Cardiac Arrest (SCA - 85% of all arrests). Well done NSW Health this has shown leadership and resolve to implement this regime in the face of biased resistance from certain quarters.
Early-onset pneumonia following bag-mask ventilation versus endotracheal intubation during cardiopulmonary resuscitation: A sub study of the CAAM trial
Josefine S Baekgaard, Mohamed N Triba, Morgane Brandeis, Jacob Steinmetz, Yves Cohen, Judith Gorlicki, Lars S Rasmussen, Sandrine Deltour, Frédéric Lapostolle, Frédéric Adnet
Resuscitation 2020, 154: 12-18
AIM: Early-onset pneumonia (EOP) is a common in-hospital complication in survivors of out-of-hospital cardiac arrest. In this sub-study of the CAAM trial, we aimed to compare whether bag mask ventilation (BMV) compared to endotracheal intubation (ETI) performed during cardiopulmonary resuscitation increases the risk of developing EOP.
METHODS: Adult patients from the CAAM trial that survived beyond 12 h of hospitalization were included. Information about in-hospital management and outcome of study subjects was systematically collected. Our primary aim was to compare the incidence of EOP in the BMV and ETI group using a series of bivariate analysis adjusting for one variable at a time and a logistic regression controlled for survival beyond 96 h, age, gender, catecholamine administration, no flow time, and initial shockable rhythm.
RESULTS: Of 627 patients from the CAAM trial that survived to hospital admission, 409 patients were hospitalized beyond 12 h and thus included (202 randomized to BMV and 20 7 randomized to ETI). Patients in the BMV group had a significantly longer period of unsecured airway during prehospital cardiopulmonary resuscitation (BMV (median): 33 min; ETI (median): 17 min, p < 0.0001). No significant difference in the development of EOP according to airway management was identified on univariate analysis (BMV: 53%, ETI: 53%, Odds Ratio 1.0 [0.7-1.5], p = 1.0). We found no difference in the development of EOP according to airway management in the series of bivariate analyses or in the multivariable regression analysis either.
CONCLUSION: In this sub-study of the CAAM trial, development of early-onset pneumonia in out-of-hospital cardiac arrest survivors did not depend on airway management technique during CPR.
ARAN Comment – Done well, ventilation in OHCA using a BVM is safe in the absence of a secured airway. The same cannot be said for BLS ventilations without a BVM.
Josefine S Baekgaard, Mohamed N Triba, Morgane Brandeis, Jacob Steinmetz, Yves Cohen, Judith Gorlicki, Lars S Rasmussen, Sandrine Deltour, Frédéric Lapostolle, Frédéric Adnet
Resuscitation 2020, 154: 12-18
AIM: Early-onset pneumonia (EOP) is a common in-hospital complication in survivors of out-of-hospital cardiac arrest. In this sub-study of the CAAM trial, we aimed to compare whether bag mask ventilation (BMV) compared to endotracheal intubation (ETI) performed during cardiopulmonary resuscitation increases the risk of developing EOP.
METHODS: Adult patients from the CAAM trial that survived beyond 12 h of hospitalization were included. Information about in-hospital management and outcome of study subjects was systematically collected. Our primary aim was to compare the incidence of EOP in the BMV and ETI group using a series of bivariate analysis adjusting for one variable at a time and a logistic regression controlled for survival beyond 96 h, age, gender, catecholamine administration, no flow time, and initial shockable rhythm.
RESULTS: Of 627 patients from the CAAM trial that survived to hospital admission, 409 patients were hospitalized beyond 12 h and thus included (202 randomized to BMV and 20 7 randomized to ETI). Patients in the BMV group had a significantly longer period of unsecured airway during prehospital cardiopulmonary resuscitation (BMV (median): 33 min; ETI (median): 17 min, p < 0.0001). No significant difference in the development of EOP according to airway management was identified on univariate analysis (BMV: 53%, ETI: 53%, Odds Ratio 1.0 [0.7-1.5], p = 1.0). We found no difference in the development of EOP according to airway management in the series of bivariate analyses or in the multivariable regression analysis either.
CONCLUSION: In this sub-study of the CAAM trial, development of early-onset pneumonia in out-of-hospital cardiac arrest survivors did not depend on airway management technique during CPR.
ARAN Comment – Done well, ventilation in OHCA using a BVM is safe in the absence of a secured airway. The same cannot be said for BLS ventilations without a BVM.
The efficacy and usability of suction-based airway clearance devices for foreign body airway obstruction: a manikin randomised crossover trial.
Resuscitation Plus Volume 5, March 2021, 100067
Resuscitation Plus Volume 5, March 2021, 100067
A new study has directly compared LifeVac with both Abdominal Thrusts (the primary first-aid measure for choking recommended by ILCOR) and the Dechoker device. The study found that for the primary outcome, the FBAO was successfully removed in 99% cases with LifeVac, 74% cases with Dechoker, and 71% cases with abdominal thrusts . The odds of successful removal was significantly higher in the LifeVac group than abdominal thrusts but was not significantly higher in the Dechoker group compared with abdominal thrusts.